Author: schcc
COVID-19 After Action Review
SCWIHERC will be hosting a COVID-19 After Action Review on September 22.
SCWIHERC COVID-19 AAR Meeting
SCWIHERC will be hosted a COVID-19 After Action Review on September 22. The After Action Report and Improvement Plan will be available soon.
May 3, 2021 Meeting
SCWIHERC General Membership Meeting May 3, 2021 Notes
Meeting recording (expires May 3, 2022): https://transcripts.gotomeeting.com/#/s/f3033c32f10107e293a0e392234b83295b8894a7706f834d9982d77fef8671c8
Intro updates and reminders:
SCWIHERC is seeking nominations for a hospital representative on our Board of Directors. Nominations should be sent to jennifer.behnke@scwiherc.org by May 17.
SCWIHERC still has UV lights disinfection lights available to partners, reach out to jennifer.behnke@scwiherc.org for more info.
Katherine Johnson, WI DHS OPEHC Systems Coordinator, gave an update on several platforms and projects:
EMResource: SNFs have been built in EMResource and we are working to engage them to have them update their bed availability weekly or as it changes. This was a lesson learned during the pandemic with discharging patients needing post-acute care, and the hope is that this will be an up to date resource that hospital discharge planners can use to find open beds while benefitting SNFs who have open beds. This webinar was recorded to show SNF users the system: https://livestream.com/accounts/14059632/events/9579680/videos/218837973
Event response has been somewhat poor recently, including for real events. Please check your alerts and ensure your phone is confirmed to receive text alerts. We are looking at bringing on voice alerts, which enable the system to robodial any phone number to indicate there is an event going on. This would be particularly beneficial for organizations that carry phones that do not receive text messages.
EMTrack, the patient tracking software, and eICS, incident management software for the HERCs are both expected to go live soon and more information will be coming. This link provides a demo on how EMTrack works: https://transcripts.gotomeeting.com/#/s/33895863d0031880b55f29b72d09045de0f01423fa22932eb66a5bb177404558
WISCOM: WI DHS had a funding opportunity to provide updated type 1 WISCOM radios to all hospitals in the state at no cost to the hospitals. See separate email on May 3 from Jennifer for a flyer with details. Hospitals will be asked to provide a contact where the WISCOM agreement should be sent for signature via Docusign if they wish to receive the new equipment.
We had an open discussion on COVID-19 including strategies for reaching those still unvaccinated. Partners are using different approaches including walk in clinics, flexible clinic hours, targeting outreach to include the homebound, vulnerable, BIPOC communities, using creative venues including parks, malls, job centers, workplaces to meet people where they live, work, and play. Some are holding local vaccinator coordination meetings to guide their planning and improve equity. Business partnerships that were forged during previous outbreaks are now being leveraged to offer vaccine clinics for their workforce.
We reviewed existing SCWIHERC plans and our Health Emergency Planner, Amanda Hauser, gave an overview of the new state and regional burn plans. The burn plans detail how we plan to coordinate and provide care to patients for up to 72 hours in the event of a burn mass casualty incident if the burn centers in the state (UW Health and Columbia St. Mary’s Milwaukee) are already full, and burn victims have to be cared for at all trauma centers (including level I, II, III and IV) until they can be transferred to burn centers in the state or out of the state if needed. Level II trauma centers are asking to serve as burn surge facilities and will hear from us separately on what that entails. Level III and IV trauma centers are being asked to facilitate several RNs, an ED physician, and a general surgeon receive ABLS Now training to be able to provide this care. WI DHS and SCWIHERC have some funding to support the provision of this training.
All SCWIHERC plans can be found in the SCWIHERC shared drive. They were recently updated for the year and we are seeking feedback on them; after they are finalized, we will be asking our partners to sign off acknowledging these plans. See separate email from Jennifer for more information.
SCWIHERC still intends to host a COVID-19 AAR in late summer, hopefully in person! SCWIHERC also intends to host a Healthcare Recovery TTX in the fall, rescheduled from spring 2020.
Meeting attendance:
Kurt Hoeper- Upland Hills Health
Charlie Johnson- SSM Health Waupun
Jodi Moyer- Beloit Health System
Tina Strandlie- Stoughton Health
Laura Kane- UW Health
Eric Anderson- Dane County EMS/EM
Ben Eithun- SCWIHERC and UW Health
Alesha Erdenberger- Care and Rehab
Terra Whirry- Columbia County HD
Tanna McKeon- Green Co EM
Sam LaMuro- Fort Health Care
Josh Kowalke- Reedsburg Area Ambulance
Kara Takes- Unified Therapy
Julie Staffin- Mayville EMS
Jen Weadge- Rock Co HD
Aurielle Smith- PH Madison and Dane County
Mary Tessendorf- Monroe Clinic
Erin Francois- New Glarus Home
Christal Foreyt- Gundersen Boscobel
Dave Kitkowski- St. Clare Baraboo
Gail Scott- Jefferson Co HD
Alison Hanamann- Edgerton Hospital
Amanda Gessler- St. Mary’s Madison
Jeff Kindrai- Grant Co HD
Amy Nehls- Dodge County EM
Leslie Cody- Allay Hospice
Asa Rowan- Beloit Area Community Health Centers
Angie Cohen- Grant Regional Health Center
David Drews- Columbia Co
Belle Koch- Sauk Prairie Hospital
Ed Somers- Clearview Dodge Co
Sharon Warden- Mile Bluff Medical Center
Sally Blackbourn- Memorial Hospital of Lafayette Co
Diana Quinn- SSM Health
Ron Krause- Mercyhealth
Suzanne Schreiner- Adams Co HD
Brian Allen- Southwest Health
Shelly Beschta- Reedsburg Area Medical Center
Christa Drays- Rainbow Hospice
Steve Haskell- UW Health
Dawn Eskau- Marquette Co HD
Mike Hall- Monroe Clinic
Bob Swenarski- St. Mary’s Janesville
Bill Ritzer- Reedsburg Area Medical Center
Kathy Johnson- Columbia County EM
Emily Kosterman- Waupun Memorial Hospital
Sharon Rateike- St. Mary’s Janesville
Carol Brown- Rainbow Hospice
Debbie Siegenthaler- Iowa Co HD
Jane Gervais- Adams Co EM
Ann Zenk- Wisconsin Hospital Association
Stephanie Kuschel- Mercyhealth
Kevin Weber- Sauk Prairie Ambulance
Ben Ruyle- St. Clare Baraboo
Heather Poker- St. Mary’s Madison
Jodie Molitor- Sauk Co HD
Erin Hastert- Lafayette Co HD
Tammy Kingery- Gunderson Moundview
Jennifer Vosen- Sauk Co Health Care Center
Nathan Bubenzer- Meriter UPH
Donna Haugom- Jefferson County EM
Dave Larson- Madison VA
Carrie Meier- Dane County EM
Alison Chouinard- Rock Co HD
Jessica Lake- FBI
Carmen Luther- Reedsburg Area Medical Center
Michael Niles- Rock Co HD
Karen Sell- Prairie Ridge Health Columbus
Katherine Johnson- WI DHS OPEHC
Amanda Hauser- WI DHS OPEHC
Jennifer Behnke- SCWIHERC
November 4, 2020 Meeting
SCWIHERC General Membership Meeting November 4, 2020 Notes
Meeting recording (expires May 4, 2021): https://transcripts.gotomeeting.com/#/s/d6b15298f36934f6312486e2957d822d8628f6199003b08f25da175c27eea927
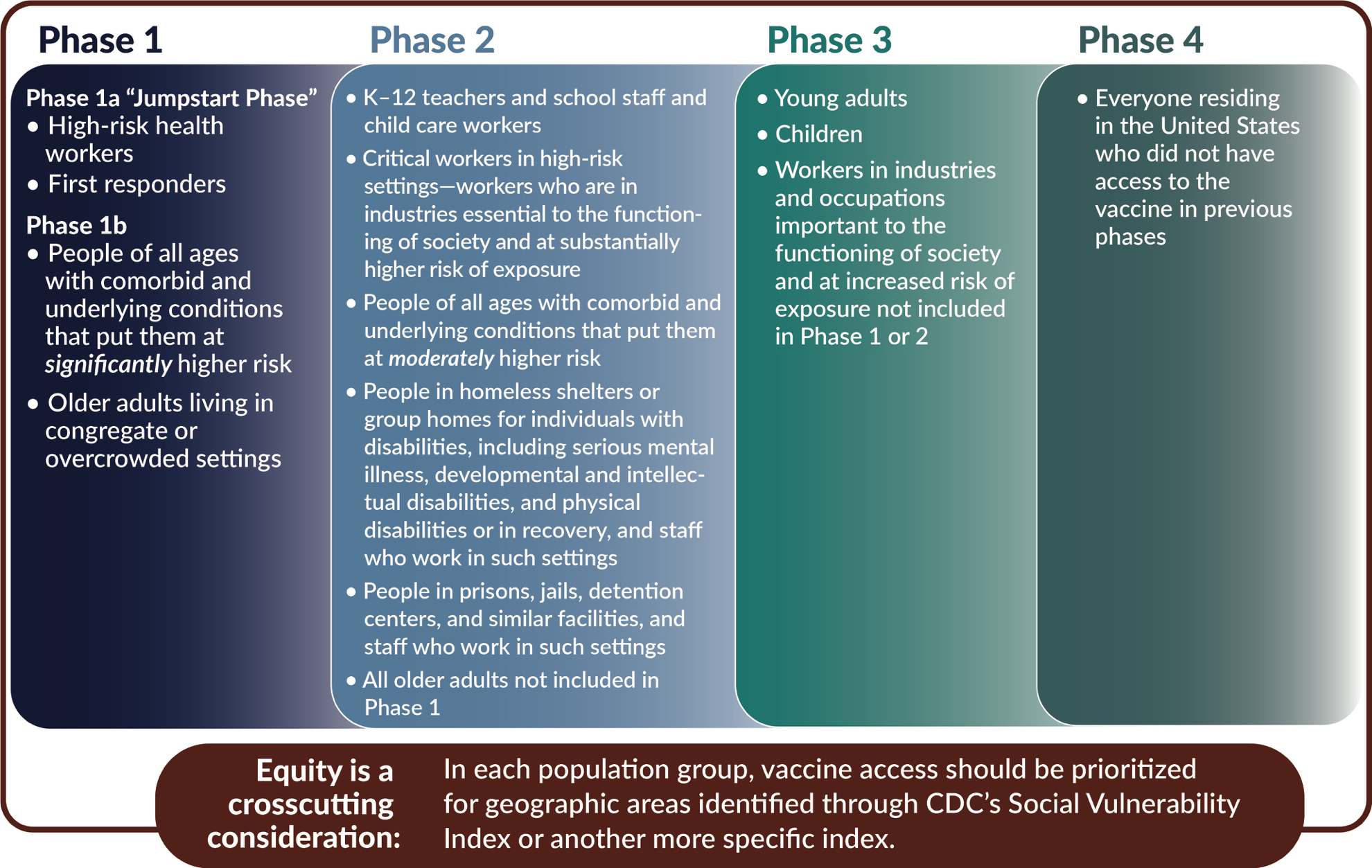
Doug Hill gave an update on COVID-19 Crisis Standards of Care, including the work being done by the State Disaster Medical Advisory Committee (SDMAC). The state is expected to release guidance that mimic’s that of the National Academy of Medicine for COVID-19 vaccination priority groups. Refer to the following documents:
Framework for Equitable Allocation of COVID-19 Vaccine from the National Academy of Medicine:
https://www.nap.edu/read/25917/chapter/1
This figure is on page 30 of the PDF. Wisconsin’s guidance is likely to mirror this approach:
(Share Ethical standards document here)
Kevin Wernet gave an update on Mortuary Affairs and mass fatality planning. Key points:
Reach out early to your local EM if you have needs (body bags, cold trailers)
Observe practices that respect the decedent.
Move decedents out of their unit bed. If there is no room in your morgue, consider meeting the funeral home director at an entrance rather than bringing them into your facility and onto the patient care units. Leaving the decedent on the unit and having the funeral home pick up from the unit directly increases their exposure and PPE burn rate.
Kevin also gave an update from the PPE task force.
Key message: every N95 mask that is discarded instead of decontaminated is one less mask we have during this pandemic and for flu season. If internal resources are not available for decon, everyone is eligible to use the Battelle System.
See Respirator Reuse Guidance: https://www.dhs.wisconsin.gov/publications/p02699.pdf
Email Kevin with any questions on these topics: kevin.wernet@wisconsin.gov
Updates
Hospitals- please fill out the Match survey to capture hospital involvement in real events and exercises. It takes about 10-15 minutes if you have your AAR handy. We use this information to capture your in-kind efforts to meet our required 10% match of our federal grant. Link: https://www.surveygizmo.com/s3/3321278/WHEPP-Exercise-and-Real-Event-Report-F-02007-01-2017
SCWIHERC COVID-19 Mass Vaccination Functional Exercise is rescheduled for December 9, deadline to register is November 25. To be determined if we will have a spring exercise. Healthcare Recovery TTX that was originally scheduled for spring 2020 may be postponed to fall 2021 depending on vaccination efforts.
We are offering a virtual condensed public information officer 4 hour course soon. This course does not replace the G290 PIO curriculum (a 16 hour course), but offers a training for partners in PIO roles that have not been able to take formal training. The goal is to balance current demands due to COVID surge with the need to deliver this course in time to use the skills learned when communicating with the public regarding COVID-19 vaccination efforts. We conducted a poll during the meeting to determine when to schedule the course. Update: January was the top choice, we are looking at scheduling in early-mid January.
There are also many virtual training offerings available to keep up on your skills and knowledge since we cannot offer in-person trainings at this time. Refer to
Center for Domestic Preparedness Virtual Instructor-Led Training: https://cdp.dhs.gov/vilt
Wisconsin Emergency Management virtual offerings (in purple): https://www.trainingwisconsin.org/Schedule.aspx
The list produced by Svea Erlandson and Mariel Torres, our WI DHS Training and Exercise Coordinator and Specialist.
HERC Virtual Training Resources
We resumed our weekly SCWIHERC COVID-19 discussion and gave organizational updates.
Meeting attendance:
Brad Armstrong, UPH Meriter
Diana Quinn, SSM Health
Jodi Moyer, Beloit Health Systems
Nathan Bubenzer, UPH Meriter
Sharon Warden, Mile Bluff Medical Center
Alice Salli, Mendota Mental Health Institute
Alison Chouinard, Rock Co Health Dept
Angie Cohen, Grant Regional Health Ctr
Ben Eithun, UW Health/AFCH/SCWIHERC
Bill Ritzer, Reedsburg Area Medical Center
Brian Allen, Southwest Health
Carrie Meier, Dane County EM/EMS
Dave Larson, Madison VA
Deanna Wright, Memorial Hospital of Lafayette Co
Debbie Siegenthaler, Iowa County Health Dept
Diana Arneson, Rock County
Donna Haugom, Jefferson County EM
Gail Scott, Jefferson Co Health Dept
Steve Haskell, UW Health
Jane Gervais, Adams Co EM
Jodie Molitor, Sauk Co Health Dept
Jon Erdmann, Divine Savior
Josh Kowalke, Reedsburg Area Ambulance
Julie Leibfried, Lafayette Co Health Dept
Kacey Kronenfeld, Madison Emergency Physicians
Kate Stauffacher, Recover Health
Ken Kaiser, Grant Regional Health Ctr
Brenda Koehler-Borchardt, Watertown Regional Medical Ctr
Kristin Osterday
Laura Kane, UW Health
Leslie Cody, Allay Home and Hospice
Lisa Herritz, Ho Chunk Nation Health Dept
Patrick Monckton, Southwest Health
John Pettey, St. Mary’s Madison
Bob Swenarski, St. Mary’s Janesville
Sally Blackbourn, Memorial Hospital of Lafayette Co
Sam LaMuro, Fort Health Care
Sharon Foley, Divine Savior
Stephanie Novak, Marquette Co Health Dept
Tina Strandlie, Stoughton Hospital
Anna Taylor, Monroe Clinic
Carmen Luther, Reedsburg Area Medical Center
Lyle Kratochwill, Richland Hospital
Ashley Vickers, Mercy Walworth
Mary Crowley, Juneau County Health Dept
Guests: Doug Hill, WI DHS Crisis Standards of Care; Kevin Wernet, Wisconsin Emergency Management
Facilitated by Jennifer Behnke
SCWIHERC COVID-19 Mass Vaccination Exercise
SCWIHERC hosted a COVID-19 Mass Vaccination Exercise on December 9. The After Action Report and Improvement Plan is available here:
SCWIHERC Mass Vax POD AAR IP
Request for Proposal: Points of Dispensing Functional Exercise and COVID-19 After Action Review
SCWIHERC is seeking proposals for two separate events: a points of dispensing functional exercise and a COVID-19 After Action Review.
If you are interested in submitting an RFP, please see the attached documents and submit proposals electronically to Jennifer Behnke by close of business, July 8, 2020. Entities wishing to be considered for both exercises should submit separate proposals for each exercise.
Points of Dispensing RFP:
POD FE RFP
COVID-19 After Action Review RFP:
COVID-19 AAR RFP
Infection Control Blog
This page is a pilot project of SCWIHERC and will be used to list all infection control/outbreak notices that SCWIHERC receives, including from the Centers for Disease Control and Prevention.
All notices will be removed after 90 days unless SCWIHERC receives notice that the notice is ongoing.
Please send any feedback or questions to Jennifer Behnke
Ongoing- COVID-19 CDC and WI DHS pages
To receive SCWIHERC updates related to COVID-19, subscribe to our mailing list.
March 5, 2020 Meeting
Join us for our March 5 meeting, see the agenda for details:
Recording available until September 6, 2020: https://transcripts.gotomeeting.com/#/s/67b8068bf4188a54d212fee56709134c0d2a1faef818fe85a53ef4ed29a0922a
Reminders:
See separate trainings list for upcoming trainings.
Please monitor WISCOM HRCRD5 open/clr at all times. WISCOM should be used to verbalize EMResource/WI Trac alerts for redundancy.
Please remember to submit the MATCH survey for all hospital-based exercises and real events using this link:
We had an in-depth discussion about COVID-19 Preparedness and Response. WI DHS created a survey to assess the PPE situation for all partners in the state, and this survey data is being shared with federal partners to assess the need to mobilize stockpiles, so please fill out the survey emailed out by Jennifer. Please find the one best representative in your facility to respond to the survey to avoid conflicting duplicate survey responses. Feel free to fill out the survey multiple times if the PPE situation in your organization changes. The SCWIHERC COVID-19 briefings will continue weekly until further notice.
The next portion of the meeting was dedicated to the Coalition Surge Test After Action Review and Facilitated Discussion. This information can be found in the after action report when available.
The Hospital and Medical Surge workgroups met in the afternoon and discussed surge planning in response to respiratory virus season and COVID-19, as well as MCI readiness. Three resources were shared by Jennifer:
CDC Mass Casualty Predictor Model
https://hsdl.org/?view&did=24463
Trauma centers: Prepare for mass casualty incidents by understanding the 10 predictable stages of disruption
Strategies for Improved Hospital Response to Mass Casualty Incidents
Meeting attendance:
Ashley Buys- UW Health
Jacob Greenberg- UW Health
Mary Crowley- Juneau Co HD
Lisa Herritz- Ho Chunk Nation HD
Laura Kane- UW Health AFCH
Asa Rowan, Community Health Systems
Sheryl Krause- Fort Healthcare
Brenda Koehler-Borchardt- Watertown Regional Medical Ctr
Jeff Kindrai- Grant County HD
Thomas Ellison- UW Health
Joe Meagher- Dodge Co EM
Amy Nehls- Dodge Co EM
Dave Larson0 Madison VA Hospital
Jane Gervais- Adams Co EM
Samantha Marcelain- Gundersen Moundview
Christal Foreyt- Gundersen Boscobel
Joni Marty- Green Co HD
Alison Chouinard- Rock Co HD
DeAnn McAllan- American Red Cross
Mary Tesserdorf- Monroe Clinic
Jodi Moyer- Beloit Health System
Johnny Holt- St. Clare Baraboo
Jon Erdmann- Divine Savior
Sharon Foley- Divine Savior
John Rago- Baraboo EMS
Julie Gorman- Sauk Prairie Healthcare
Abigail Kuehn- Watertown HD
Victoria Parker- Watertown HD
LuAnn Reuter- Prairie Ridge Health
Karen Sell- Prairie Ridge Health
Kyle Schaefer- UW Health
Jeff Ethington- UW Health OPO
Julie Muhle- Marshfield Medical Center Beaver Dam
John Pettey- St. Mary’s Madison
Jennifer Behnke- SCWIHERC
Online:
Dave Kitkowski- St. Clare Baraboo
Tana Buss- UW Health
Emily Kosterman- Waupun Memorial
Sue Matye- Iowa Co HD
Tanna McKeon- Green Co EM
Stephanie Kuschel- MercyHealth Janesville/NIPARC
Jen Boigenzahn- Gundersen
Carol Brown- Rainbow Hospice
Sarah Hughes- PH Madison Dane Co
Kathy Noe-
Sharon Rateike- St. Mary’s Janesville
Patrick Monckton- Southwest Health
Brian Allen- Southwest Health
Erin Hastert- Lafayette Co HD
Angie Cohen- Grant Regional Health Center
November 20, 2019 Meeting
November 20, 2019 Membership Meeting Notes
SCWIHERC Updates:
As of October 23, SCWIHERC is incorporated, now we are seeking nonprofit status to help support our long-term sustainability.
Our spring tabletop exercise topic is healthcare system recovery. The scenario will be written to engage all core partners: hospitals, public health, EMS, emergency management, and other healthcare providers. Tentative dates are April 14-16. We need exercise design team members, please let Jennifer know if you are interested in being on the design team.
The coalition surge test will be taking place again in late winter. We need to simulate evacuation of 430 patients to meet our 20% surge threshold required by our grant. If you are interested in volunteering to be an evacuating hospital, please let Jennifer know. If we do not have enough volunteers, we will ask hospitals directly to meet our federal requirements.
A training matrix was distributed listing all upcoming trainings for the remainder of the grant year. That information is summarized here: http://www.scwiherc.org/category/training/http://www.scwiherc.org/category/training/
CORRECTION: the training matrix had an error, the PER 211: Medical Management of CBRNE Incidents is May 18-19, NOT May 17.
Tracey Froiland, Fox Valley HERC Coordinator, presented on their Infectious Disease Go-Team. They pioneered this novel concept of forming a team to care for high consequence infectious disease patients in their home using telemedicine. This specially-trained team can also support caring for these patients in a hospital setting. See their promotional video for more info: https://www.youtube.com/watch?v=L4O3ZWkJgJ8
Tracey’s slides will be available in the SCWIHERC shared drive soon.
We had several partners present on different organizations that provide human personnel assets used in response. Presentation highlights:
WEAVR- Wisconsin Emergency Assistance Volunteer Registry: https://weavrwi.org/
Individual registry- Wisconsin’s ESAR-VHP. A database of individuals who can support the health needs of an incident. Pre-registered individuals have been vetted through a background check and credential verification. Individuals who are registered in WEAVR and deployed through a WEAVR request during a federal or state declared emergency are offered liability protection through Wisconsin Statute 257. The state is seeking clarification from the Office of Legal Counsel on whether this liability protection is available in the absence of federal or state declaration.
Registration in WEAVR is not a commitment to serve in any emergency. Please encourage your staff and partners to register!
MRC- Medical Reserve Corps. Brenda Lutz-Hanson presented on the Region 4 MRC and the purpose, mission, and sustaining of MRCs in Wisconsin. The entry point for MRCs in Wisconsin is registering in WEAVR and selecting the affiliation with an MRC. Currently, Region 5 (SCWIHERC’s region) has no active MRCs. Managing an MRC is often, but not always, done by local health departments. There is some work involved, but federal grant dollars may be available to support this effort. Contact Jennifer for more information.
DMAT- Wisconsin’s Disaster Medical Assistance Team. Patty Scanlin presented on this asset. They deploy outside of Wisconsin to assist medical operations after disasters and for large, planned events such as presidential funerals or inaugurations. They have field hospital capabilities. DMAT personnel are vetted by the federal process that takes 1-2 years and train on personal time, but are paid during deployment. Deployment notice may be as short as 12-24 hours, and deployments can last from 10-14 days.
American Red Cross- Connie Miley spoke about the volunteer capabilities and opportunities with American Red Cross. They often support sheltering and mass care operations all over the state and country.
Team Rubicon- Jodi Moyer spoke the mission and capabilities of Team Rubicon. They deploy nationally and focus on debris cleanup but have other capabilities. They are a veteran founded organization and 75% of their volunteer force is veterans. They are supported by donations from individuals and companies, and receive no payments by individuals impacted by disasters.
A question came up about requesting and utilizing any of these resources. It is strongly recommended that all requests are made through local emergency management. This helps ensure that those affected receive the most appropriate resource for their needs, and also may have reimbursement ramifications if federal or state funding is available for incident response and/or recovery.
Svea Erlandson, WI DHS Training and Exercise Coordinator, facilitated our Training and Exercise Planning Workshop in the afternoon. We reviewed data from the training needs assessment survey, and then had a productive conversation about developing training priorities and how to support these with available trainings. The three training priorities identified included Ensuring the Continuity of Healthcare Service Delivery, Catastrophic Event Preparedness for the Health Sector, and Health Emergency Management Orientation for partners in Wisconsin. These priorities will guide trainings offered in the July 1, 2020 to June 30, 2021 grant year.
Our meeting concluded with discussion on special populations and triaging the most important needs according to life safety priorities.
Grant guidance on this topic: Support HCC members with situational awareness and information technology (IT) tools already in use that can help identify children, seniors, pregnant women, people with disabilities, and others with unique needs. Support HCC member agencies in developing or augmenting existing response plans for these populations, including mechanisms for family reunification. Identify potential health care delivery system support for these populations (pre- and post-event) that can prevent stress on hospitals during a medical surge event. Assess needs and contribute to medical planning that may enable individuals to remain in their residences during certain emergencies. When that is not possible, coordinate with the jurisdiction’s ESF-8 lead agency to support the jurisdiction’s ESF-6 (Mass Care, Emergency Assistance, Housing, and Human Services) lead agency with access to medical care including at shelter sites. Coordinate with the jurisdiction’s ESF-8 lead agency to assess medical transport needs for these populations.
Jennifer also offered a definition for those with access and functional needs according to FEMA: Children and adults with physical, mobility, sensory, intellectual, developmental, cognitive, or mental health disabilities. Older adults. People with temporary or chronic health conditions (including taking daily medication). Women in late stages of pregnancy. People needing bariatric equipment. People with limited English proficiency, low literacy, or additional communications needs. People with very low incomes. People without access to transportation. People experiencing homelessness.
Based on this guidance and definition, the group identified these most urgent life safety priorities:
Electricity dependent individuals- how to find them before the incident, how to empower them to prepare for a power outage, how to care for them during a power outage, and how to partner with other groups to support these three capabilities. This includes home health, durable medical equipment suppliers, primary care providers.
Individuals with unreliable transportation options- planning for those who need transportation assistance for their medical appointments, and for those who don’t have the transportation means to evacuate when a community evacuation is ordered.
Individuals on medications for medical conditions- helping these individuals maintain an adequate supply of medications before an incident so they don’t run during an incident when normal suppliers may be disrupted, or if they cannot travel to refill meds. This includes working with other healthcare providers to share this message with vulnerable patients.
Supporting Home Health Agency Continuity of Operations- recognizing that HHAs are critical to keeping individuals with various conditions healthy and able to live at home, we will look for ways to support HHA continuity of operations so they can continue to do what they do every day even after a large or disruptive incident.
Meals on Wheels- supporting these agencies that meet the basic dietary needs of vulnerable individuals on a daily basis so that they can continue this important mission even after incidents.
Supporting better communications for these special populations, including the English as a second language community and those with low literacy levels. Not only translating written materials and having sufficient interpreter services available for every step of preparedness, response, and recovery, but also utilizing multiple channels of information dissemination. This can include traditional media channels like television, radio, and print, but also cultural and faith-based organizations that serve a role in gathering and outreach to these individuals and groups.
Important partners to engage in supporting these important missions can include local human services agencies, primary care organizations, home health agencies, long-term care organizations, Aging and Disability Resource Centers, WIC (Women, Infants, and Children) nutrition programs, 211 and United Way, and cultural and faith-based organizations.
The next steps proposed by the group include inviting representatives from these important partners to a round-table discussion to more thoroughly explore how we can work with these partners to promote preparedness, and support response and recovery efforts for these special populations.
Meeting Attendance:
Bob Swenarski- St. Mary’s Janesville
Juan Cullum- Mercyhealth Janesville
Jodie Molitor- Sauk County Health Dept
Alice Salli- Mendota Mental Health
Mary Crowley- Juneau County Health Dept
Lisa Herritz- Ho-Chunk Nation Health Dept
Asa Rowan- Community Health Systems Beloit
Gail Scott- Jefferson County Health Dept
Samantha LaMuro- Fort Healthcare
Mike Hall- Monroe Clinic
Kelly Pederson- St. Mary’s Madison
Nikki Salas- Watertown Regional Med Ctr
Brenda Koehler Borchardt- Watertown Regional Med Ctr
Marie-Noel Sandoval- Rock County Health Dept
Douglas MacFarlane- Crossroads Care Center of Mayville
Tina Strandlie- Stoughton Hospital
Christal Foreyt- Gundersen Boscobel Hospital and Clinics
Josh Kowalke- Reedsburg Ambulance
Jill Lenz- Columbia County Health Dept
Susan Lorenz- Columbia County Health Dept
Mike Lohmeier- SCWIHERC Medical Advisor
Carrie Meier- Dane County Emergency Mgmt
Connie Miley- American Red Cross
Jon Erdmann- Divine Savior Healthcare
John Longo- WI DHS OPEHC
Tracey Froiland- FVHERC
Mike Stephens- UW Health
Sarah Mattes- Public Health Madison Dane County
Steve Haskell- UW Health
Patricia Scanlin- UW Health TAC, WI DMAT
Sharon Foley- Divine Savior Healthcare
Alison Chouinard- Rock County Health Dept
Julie Muhle- Beaver Dam Marshfield Medical Center
Marla Noordhof- Beaver Dam Marshfield Medical Center
Abbey Kuehn- Watertown Health Dept.
Sarah Stewart- Watertown Health Dept
Dan Michaels- Public Health Madison and Dane County
Dave Larson- Madison VA Hospital
Joe Meagher- Dodge County Emergency Mgmt
Jodi Moyer- Beloit Health System
Nathan Bubenzer- Meriter UnityPoint Health
Sue Matye- Iowa County Health Dept
Karen Sell- Prairie Ridge Health Columbus
Amy Hollis- Monroe Clinic
Svea Erlandson- WI DHS OPEHC
Brenda Lutz-Hanson- La Crosse County Health Dept
Jeff Ethington- UW Health OPO
Jennifer Behnke- SCWIHERC
September 10, 2019 Workgroup Meeting- Spec Path, PHEP, Spec Pop
9-10-19 Special Pathogens, PHEP, Special Populations Workgroup Meeting
General
Reminder that the Closed POD workshop is September 26. Formal registration is closed but Jennifer can still add a few attendees, email her for last minute registrations.
The plan for the next meeting includes an infectious disease go team presentation, human personnel assets (WEAVR, MRC, DMAT) presentation, Training and Exercise Planning Workshop, workgroups. It wiill consume most of work day but we will provide lunch, partners are welcome to come and go. Looking at November 20, somewhere in the Madison area.
We talked about hosting a communications workshop covering the topics of social media, media relations, Joint Information Systems operations, organizational internal communications (with staff/patients), message mapping. Partners agreed this is a good topic.
We talked about the opportunity for a healthcare recovery/continuity of operations tabletop exercise, which is strongly suggested in the grant language: Supporting member organizations in defining what their “essential functions” that must be maintained after disruption of normal activities and determining priority for restoration if compromised and determining what the coalition might do to assess and support the maintenance of these functions. Admin/Finance operations, Supply Chain, Shelter in place, staff support and resilience including mental health support. Suggested to add a 96-hour sustainability plan component. This is distinct from the business continuity planning workshop offered in April, as we will be more formally exploring how an emergency disrupts healthcare delivery, how we assess essential services and how to prioritize restoring them, and how SCWIHERC can assist this effort. Targeted audience includes all coalition disciplines.
We also talked about the opportunity for a communications workshop and what our current gaps are that should be addressed by this. We came up with social media, media relations, Joint Information Systems operations, organizational internal communications (with staff/patients), and message mapping. There is a vendor used by another region that conducts customized workshops on these topics and this could be an opportunity, especially if we can invite members of the media for a meet and greet to build relationships before incidents happen. A suggestion was made to include other media outlets (TV/radio/newspaper) outside the Madison market in addition to the Madison market.
Reminder that the Coalition Surge Test will also be an exercise this year.
SCWIHERC scholarship opportunity announcement coming soon. Public health partners are asked to utilize PHEP funding instead, they will have funding comparable to last year for scholarships.
The goal for all workgroups is to define goals and objectives, nominate a leader, share lessons learned, and make progress on grant requirements relevant to the workgroup.
Special Pathogens Discussion
Grant guidance on this topic:
Educate stakeholders on current policies and practices regarding the type of PPE necessary for various infectious pathogens, and the availability of PPE resources, to include stockpiling considerations, vendor-managed inventories, and the potential for reuse of equipment.
During an infectious disease outbreak, ASPR and CDC require that recipients and HCCs coordinate the following activities to ensure the ability to surge to meet the demands during a highly infectious disease response: Establish a Medical Common Operating Picture, Develop or update plans accordingly, Establish key indicators and EEIs, Provide real-time information sharing, Coordinate public messaging.
Support and promote regional PPE procurement, Equip, train, and provide resources necessary to protect responders, employees, and their families from hazards during response and recovery operations. PPE, MCMs, workplace violence training, psychological first aid training, others.
We discussed the special capabilities of certain organizations in our region related to handling patients with high consequence infectious diseases (HCID). Nomenclature note: while these capabilities were built using support and guidance prescribed by the Ebola grant administered through ASPR/HPP, we have updated the preparedness and response activities to encompass all high consequence infectious diseases.
UW Hospital is a category 1 Ebola Treatment Facility. Their activities and capabilities include the ability to treat up to 2 confirmed HCID/Ebola patients at a time. They support this through their HCID team which includes representatives from infection control, infectious disease, emergency medicine, and others. They do quarterly training and a required annual HCID drill with performance measures reported to the feds.
St. Mary’s Madison is a category 2 Assessment Facility. Under ideal circumstances, if public health is alerted to a potential HCID patient, they are directed to St. Mary’s rather than presenting at their preferred hospital or clinic. Their activities and capabilities include being able to admit and treat a suspected HCID/Ebola patient for up to 72 hours, the window it could take to receive confirmed positive laboratory results for a patient. If the patient is confirmed positive, they are transferred to a treatment facility, which could include UW Hospital or the regional treatment center, which is the University of Minnesota Medical Center West Bank. St. Mary’s does quarterly training and a required annual HCID drill with performance measures reported to the feds.
The University of Minnesota Medical Center West Bank is the region’s treatment center (referring to HHS/FEMA regions, not HERC regions) and has greater capacity for HCID patients than UW Hospital.
It is protocol for a confirmed positive patient to be transferred to UMMC West Bank. Situations that would alter this protocol include if the patient was not stable enough for transfer, terminally ill, or if UMMC West Bank’s HCID unit was full.
Transportation of a confirmed positive HCID patient must be done by agencies that are specially trained and have HCID plans and procedures. Madison Fire has the capability to transfer within Dane County, and Baraboo EMS has the capability to transfer anywhere within Wisconsin and from anywhere in Wisconsin to UMMC West Bank.
Baraboo EMS has a cache of PPE, two ISO PODS, and procedures for transporting a HCID patient. There is one medic donning a full PAPR who accompanies the patient (contained in an ISO POD), a driving medic that wears certain PPE, and the ambulance is followed by a chase vehicle with additional supplies that can offer support as needed. Several medics are trained in these plans and there is a very specific procedure for disinfecting the rig after transport is complete.
We were able to share lessons learned from a recent event wherein a patient with a fever of unknown origin with a positive travel history was transported by ambulance to a local facility and held until HCID was ruled out. Emphasis was placed on adhering to existing plans for these events, including prescribed communications channels.
The conversation evolved into discussion of how frontline healthcare facilities can be better prepared, and the wide assortment of PPE that is available. It was suggested that this workgroup follow up in the future with a PPE show and tell, wherein regional partners can view the different types of PPE available and perhaps move toward a goal of having the same PPE throughout the region, potentially giving us power as a region to negotiate pricing.
Many other resources were mentioned in the special pathogens discussion, listed here:
National Ebola Training and Education Center courses https://courses.netec.org/
EMS Infectious Disease Handbook https://em-ems.countyofdane.com/documents/pdf/Infection-Control-EMS-Primer-on-ID-7.11.19.pdf
WI DHS MN DPH Joint Ebola Transport Exercise Video https://vimeo.com/329950429/472b98ee2f
CDC PPE Training videos https://www.cdc.gov/vhf/ebola/hcp/ppe-training/comprehensive-ppe-training.html
High Consequence Infectious Disease Toolbox https://www.health.state.mn.us/diseases/hcid/index.html
WI DHS Disease Fact Sheets https://www.dhs.wisconsin.gov/disease/index.htm
UW Health Special Pathogens Team Blog https://spteam.uwhealth.org/
Public Health Emergency Preparedness (PHEP)
We discussed the upcoming Closed POD workshop and how SCWIHERC and the contractor are lending support, but this event will be driven by local public health partners. The event will start with a presentation on closed POD planning and logistics from Dan Michaels at Public Health Madison and Dane County, and then we will have a panel representing hospitals (Meriter), Universities (UW Madison), and private businesses (West Bend Mutual) as well as WI DHS medical countermeasures. They have a list of talking points to address including the process for creating their own closed POD plan. There will be time for Q&A from the audience. We will then break for lunch and return for a tabletop exercise on an anthrax scenario in the afternoon. Prior to the workshop, Jennifer will share the registration list, the closed POD template, and the TTX Situation Manual with public health partners for their awareness. Printed closed POD templates will be available at the workshop for reference, but local public health representatives should be the gatekeepers of the electronic template, so planning is not occurring without local public health awareness. The situation manual will be available to all partners after the exercise on the SCWIHERC shared drive, so they can use the exercise internally as they see fit.
We explored other opportunities for the PHEP workgroup to work collaboratively. It was mentioned that local public health is waiting on the state to update the PHEP plan, and the state will look into this. There was an idea to bring local public health partners together to share information and resources for completing the portions of the PHEP plan that require local customization. We will bring this idea to Southern WALHDAB for feedback.
Special Populations Discussion
This topic was unfortunately cut short due to the great conversations taking place on the previous topics.
Grant guidance on this topic:
Support HCC members with situational awareness and information technology (IT) tools already in use that can help identify children, seniors, pregnant women, people with disabilities, and others with unique needs. Support HCC member agencies in developing or augmenting existing response plans for these populations, including mechanisms for family reunification. Identify potential health care delivery system support for these populations (pre- and post-event) that can prevent stress on hospitals during a medical surge event. Assess needs and contribute to medical planning that may enable individuals to remain in their residences during certain emergencies. When that is not possible, coordinate with the jurisdiction’s ESF-8 lead agency to support the jurisdiction’s ESF-6 (Mass Care, Emergency Assistance, Housing, and Human Services) lead agency with access to medical care including at shelter sites. Coordinate with the jurisdiction’s ESF-8 lead agency to assess medical transport needs for these populations.
Jennifer also offered a definition for those with access and functional needs according to FEMA: Children and adults with physical, mobility, sensory, intellectual, developmental, cognitive, or mental health disabilities. Older adults. People with temporary or chronic health conditions (including taking daily medication). Women in late stages of pregnancy. People needing bariatric equipment. People with limited English proficiency, low literacy, or additional communications needs. People with very low incomes. People without access to transportation. People experiencing homelessness.
In planning for these populations, we talked about the need to engage more partners including home health agencies, aging and disability resource centers, family care organizations, primary care clinics, durable medical equipment companies, and 211. In the absence of comprehensive planning and up to date information, 211 can be used for just in time resource sharing to identify these populations after an event to connect them with the resources needed. Additionally, durable medical equipment companies have accurate and comprehensive lists of electricity dependent individuals, including those who have only private insurance, that can be used during emergencies.
Meeting Attendance:
Jeff Kindrai- Grant Co Health Dept
Gail Scott- Jefferson Co Health Dept
Donna Haugom- Jefferson Co EM
Alison Chouinard- Rock Co Health Dept
Kim Cox- WI DHS OPEHC
Sam LaMuro- Fort Healthcare
Brenda Klahn- St. Mary’s Janesville
Steve Haskell- UW Health
Sharon Rateike- St. Mary’s Janesville
Jony Marty- Green County Health Dept
Dave Larson- Madison VA
Anna Robb- Stoughton Hospital
Lynda Brereton- St. Mary’s Madison
Carol Quest- Watertown Health Dept
Kathy Noe- Mile Bluff Medical Ctr
John Rago- Baraboo EMS
Brad Armstrong- Meriter UPH
Nathan Bubenzer- Meriter UPH
Dan Michaels- PHMDC
Ben Eithun- UW Health AFCH
Tom Ellison- UW Health
Christal Foreyt- Gundersen Boscobel
Mike Stephens- UW Health
Juan Cullum- Mercyhealth Janesville
Mike Lohmeier- SCWIHERC/UW Health
Mary Crowley- Juneau Co Health Dept
Dave Kitkowski- St. Clare Baraboo
Alison Hanaman- Edgerton Hospital
Suzanne Schreiner- Adams Co Health Dept
Lisa Herritz- Ho Chunk Nation
John Longo- WI DHS OPEHC
Jennifer Behnke- SCWIHERC
August 27, 2019 Workgroup Meeting- Hospital, Surge, Evac, CMS
8-27-19 Hospital, Surge, Evacuation, CMS Partners Workgroup Meeting
Jennifer gave some reminders for upcoming events: SCWIHERC Closed POD Workshop September 26; Special Pathogens, Public Health Emergency Preparedness, and Special Populations Planning workgroup September 10.
We talked about the opportunity for a healthcare recovery/continuity of operations tabletop exercise, which is strongly suggested in the grant language: Supporting member organizations in defining what their “essential functions” that must be maintained after disruption of normal activities and determining priority for restoration if compromised and determining what the coalition might do to assess and support the maintenance of these functions. Admin/Finance operations, Supply Chain, Shelter in place, staff support and resilience including mental health support. We talked about how there is some overlap with the business continuity planning workshop we offered in April. We will pursue planning something like this and are looking for volunteers to participate on the exercise design team.
We also talked about the opportunity for a communications workshop and what our current gaps are that should be addressed by this. We came up with social media, media relations, Joint Information Systems operations, organizational internal communications (with staff/patients). There is a vendor used by another region that conducts customized workshops on these topics and this could be an opportunity, especially if we can invite members of the media for a meet and greet to build relationships before incidents happen. A suggestion was made to include other media outlets (TV/radio/newspaper) outside the Madison market in addition to the Madison market. We also talked about the Basic PIO course (G290) offered by Wisconsin Emergency Management. If there is enough demand for this course that exceeds local emergency management agencies’ ability to fund this course, SCWIHERC could potentially fund a course, but partners are encouraged to take advantage of the offerings on the WEM Training Portal.
We had a discussion of the history of Medical Reserve Corps groups in our region, because there are none currently active. It was suggested to have presenters come to talk about different opportunities and groups, including WEAVR, Medical Reserve Corps, and Disaster Medical Assistance Teams. This is a potential future presentation topic.
Jennifer is working on a patient tracking project with the Office of Preparedness and Emergency Healthcare along with Robert Goodland, region 1 RTAC coordinator. After an extensive review of previous pilots and current patient tracking procedures in Wisconsin, as well as best practices found in other states, there will be a patient tracking workgroup forming. We are seeking one hospital and one EMS representative from each HERC region in the state to participate in this workgroup. Jennifer will share more information about the degree of commitment involved soon. Any interested parties should reach out to Jennifer.
We had a discussion about the idea of a hospital HazMat/Decon mutual aid team. Many hospitals, especially on nights and weekends, have lean staffing that would not be able to support a complex decon operation. Additionally, clinical staff would be needed for patient care and therefore would also be unavailable. There was a mention of an initiative in another HERC region- the infectious disease mobile go team. There team has members of multiple hospitals and can deploy to the hospital or into the community to care for a patient with a high consequence infectious disease. We would like to hear more about this concept and then further discuss the possibility of a similar team trained in both HCID patient care and HazMat decon.
We discussed the SCWIHERC MCI Surge Functional Exercise held on June 19 and the AAR-IP draft that is out for review. A few improvement items were suggested:
-All situational awareness updates from an incident be communicated by WI Trac update AND by WISCOM radio update.
-Hospital staff need training in triage to manage large numbers of patients that self-present after an incident. SCWIHERC is currently developing training materials for the SALT Triage Ribbon Initiative, and we will invite local hospitals to participate in this training as well in an effort to unify EMS and hospitals in using the same triage practices.
-Hospitals need to think about perimeter control and patient access points during a mass casualty incident with large numbers of patients. All EMS transports should come one place, all untriaged patients should come to another access point where they can be separated (incident casualties versus normal unrelated ED traffic), and then casualties can further be triaged and sorted. Without a plan that addresses these issues, hospitals can very quickly deplete their staffing and resources on “green patients” (walking wounded) before they start receiving the most critically injured patients.
-Prior to a mass shooting in another area, that area cross-credentialed its clinical staff to enable them to work in other facilities. Jennifer will look into this more as a future discussion/presentation topic.
We discussed the needs of our CMS partners and how better to engage them. It was noted that they are critical in the continuum of healthcare service delivery, including helping patients to cope with emergencies and disasters so that they don’t decondition and require acute care, thereby surging local hospitals. Additionally, they can provide assistance in caring for individuals who are expeditiously discharged from hospitals (like during an emergency evacuation). There are 9 types of “CMS partners” found in Wisconsin (these are agencies affected by the CMS Emergency Preparedness Rule that was enforced starting November 15, 2017): home health agencies, skilled nursing facilities, ambulatory surgery centers, hospices, physical/occupational/speech therapy providers, end stage renal disease (dialysis) providers, federally qualified health centers, intermediate care facilities for individuals with intellectual disabilities, and critical access hospitals. It was noted that these agencies are often looking for assistance to meet their annual community-based full-scale exercise requirement. Jennifer noted that a workshop was held in Dane County last year to address this requirement, and we could potentially duplicate this effort for partners throughout the rest of the region.
Finally, we talked about planning logistics of the next workgroup meetings. Meeting quarterly seems to be a good schedule, and keeping these workgroup topics together makes sense at this time. We discussed continuing to hold meetings in a central location (Dane County) versus moving the meetings to alternating parts of the region. Those in attendance at this meeting, including partners traveling from outside Dane County, agreed that holding meetings consistently in a central location was preferred over rotating meeting locations throughout the region.
Meeting Attendees:
Sam LaMuro- Fort Healthcare
Kim Cox- WI DHS OPEHC
Christal Foreyt- Gundersen Boscobel
Tina Strandlie- Stoughton Hospital
Juan Cullum- Mercy Janesville
Bob Swenarski- St. Mary’s Janesville
Cheryl Meyer- Marquardt Home Health
Jodi Moyer- Beloit Health System
Steve Haskell- UW Health
Mike Stephens- UW Health
Nathan Bubenzer- Meriter
Dave Larson- Madison VA
Dan Michaels- Public Health Madison Dane County
Ben Eithun- American Family Children’s Hospital, SCWIHERC Chair
Tom Ellison- UW Health
Alice Salli- Mendota Mental Health Institute, Central Wisconsin Center
Jeff Ethington- UW Organ Procurement Organization
Jennifer Behnke- SCWIHERC Coordinator
Sharon Rateike- St. Mary’s Janesville
Dave Kitkowski- St. Clare Baraboo
Dan Williams- South Central Regional Trauma Advisory Council
Kyle Schaeffer- UW Health
Bill Ritzer- Reedsburg Area Medical Center
Samantha Marcelain- Gundersen Moundview
Mary Crowley- Juneau County Health Department
SCWIHERC Closed POD Workshop is September 26
Click here for information and registration
SCWIHERC Closed POD Workshop
Our Closed POD Workshop took place on September 26, thank you for making it a successful event! The after action report can be found here:
SCWIHERC Closed POD TTX AAR
If you are looking for any of the resources presented at the workshop, or would like to begin planning our organization’s closed POD, please reach out to your local health department:
Adams County 608-339-4505
Columbia County 608-742-9227
Dodge County 920-386-3670
Grant County 608-723-6416
Green County 608-328-9390
Iowa County 608-930-9870
Jefferson County 920-674-7275
Juneau County 608-847-9373
Lafayette County 608-776-4895
Madison/Dane County 608-266-4821
Marquette County 608-297-3135
Richland County 608-647-8821
Rock County 608-757-5440
Sauk County 608-355-3290
Watertown (City) 920-262-8090
A Point of Dispensing (POD) is a site for mass medication distribution in the event of a public health emergency (such as an infectious disease outbreak, natural disaster, or act of terrorism). A closed POD is closed to the public and is sponsored by an agency to distribute medication to its employees and their families, and potentially the patients they serve.
June 7, 2019 Meeting
June 7, 2019 Meeting Notes
Meeting slides:
June 7, 2019 Meeting Slides
Hospital Meeting:
Reminders and Updates: The Match Survey is due June 30 for any real events or exercises in which your hospital was a primary player/responder. We use this data to document in kind support because ASPR requires that we match a percentage of our grant funding through in-kind support. If you have your AAR handy, this should take you less than 10 minutes.
Next WISCOM roll call will be June 18, so we can do a radio check for our exercise on June 19. Jennifer will send you a heads up like usual.
We discussed the upcoming SCWIHERC MCI Surge Functional Exercise. Exercise document packets were available at the meeting for attendees. Each packet contains the ExPlan, Controller/Evaluator Handbook, the Master Scenario Events List, the Exercise Evaluation Guides, the Player Briefing, the Communications Plan, a facility sign-in sheet, a Regional Medical Coordination map, and a paper patient packet customized for each facility. The docs will also be emailed out a few days before the exercise, including the communications plan which already needs updates. If you did not attend the meeting in person, Jennifer will mail the packet to you. The controller evaluator briefing will be June 13 at 9:30, and we will have a briefing the morning of the exercise as well.
We discussed the future of the hospital workgroup. Hospital members agreed there is still value to the workgroup. We will include topics like open discussions on hospital-focused lessons learned, regulatory/accreditation compliance, and other topics that come up.
Christal Foreyt discussed the Center for Domestic Preparedness HERT course and talked about opportunities for HAZMAT training and education, and decon team recruitment. We discussed the opportunity for a HAZMAT mutual aid team when a hospital doesn’t have enough internal staff to do a large scale decon operation. We also discussed the need for hospitals to be doing decon drills with their local fire departments. The hospital workgroup will follow up on this topic in the future.
Kyle Schaefer debriefed the SIMCOM 2019 exercise. Our region did a great job responding to WISCOM roll call as part of SIMCOM, we had the highest response rate of the seven regions in the state. This roll call included flipping to the encrypted channel, and we learned a few things about how the encrypted channel works. Kyle and Bill Tyler may follow up with any information learned from the vendors on this.
Membership Meeting
Save the Date: The SCWIHERC Closed POD (point of dispensing) Workshop will be September 26. This will have a presentation on closed POD planning and operations, a panel of representatives from healthcare, a university, and a private business talking about their closed PODS including opportunities for Q&A, and a tabletop exercise with local public health reps to help facilities at all stages of the closed POD planning process.
A reminder that the SCWIHERC MCI Surge Functional Exercise is June 19. There will be many WI Trac alerts that go out that morning, apologies in advance for any alert fatigue. It should be a great opportunity to illustrate SCWIHERC response operations and the regional medical coordination plan, as well as how WI Trac supports information sharing and situational awareness during an incident.
Doodle Polls will be sent out to determine future dates for workgroup meetings. Until each meeting establishes its own agenda and meeting schedule, we will lump similarly themed workgroups to make the most of partner’s travel:
Hospital-surge-evacuation-CMS partners
Special pathogens-public health emergency preparedness (PHEP)-special populations planning.
We discussed and clarified portions of the response plan. ASPR will expect all core disciplines sign off on the plan in the future.
We discussed regional training needs. ASPR places a significant emphasis on training in the new grant, and we have to submit tentative training plans for the year to ASPR by July 31. We also discussed strategies for improving attendance at trainings, as it is not fiscally responsible to offer trainings that are less than 20% full. In the future, SCWIHERC may consider subsidizing travel to trainings to assist partners in attending. A tentative training plan was drafted based on the results of the training needs assessment conducted in late fall/winter 2018, Jennifer will coordinate with other regions to bring these trainings to our region or elsewhere in the state. See meeting slides for details.
Erica Kane from Emergency Medical Services for Children shared a presentation, including EMSC performance measure data for region 5. EMSC also has resources available for pediatric patients, such as comfort kits and pediatric prehospital care guides. Erica can be reached at ekane@chw.org and refer to the slides and their website: https://www.chawisconsin.org/initiatives/emergency-care/emergency-medical-services-for-children/
EMSC Slides
EMSC Presentation June 2019
We talked about measles preparedness for anticipated measles cases in the state. The incident/case response flowchart shared by Public Health Madison Dane County will be distributed by email to the WALHDAB group and public health representatives. We also discussed getting ahead of taking care of our first responder community and others who may be exposed without adequate PPE. All questions should be directed to your local public health officer. The WI DHS Bureau of Communicable Diseases is working on some uniform guidelines and communications resources. The most up to date information from WI DHS can always be found at https://www.dhs.wisconsin.gov/immunization/measles.htm including guidance at the bottom for public health and healthcare organizations.
Cassidy Walsh gave an introduction to the Inventory Management and Tracking System available to health departments for medical countermeasures tracking. More information is at https://www.phe.gov/about/sns/Pages/imats.aspx and in this flyer:
MCM Inventory Management and Tracking System Flyer
We introduced Kim Cox, the new HPP-PHEP program coordinator for WI DHS. She gave some updates from WI DHS including new staff and some new requirements from our new ASPR HPP Cooperative Agreement that starts July 1, 2019. Jennifer also shared some new requirements of note to the membership. See meeting slides for details.
Svea Erlandson, WI DHS State Training and Exercise Coordinator, gave the region an introduction to the Dells-Delton Area Response Exercise Series (DARES) being planned. This is WEM’s capstone exercise for 2020 (2016 was Miles Paratus, 2018 was Dark Sky). With this exercise taking place in our region, and its scenarios involving mass casualty incidents, medical surge, family assistance centers, and mass fatality management. With the unique mix of permanent residents and seasonal visitors to the Dells area, our health partners have a unique opportunity to take advantage of multiple training and exercise opportunities through this series. Contact Jennifer to see the slides shared on DARES. Svea can be reached at charlotte.erlandson@dhs.wisconsin.gov
Meeting Attendance:
Jeff Kindrai- Grant County PH
Sam LaMuro- Fort Healthcare
Gail Scott- Jefferson CO PH
Elizabeth Chilsen- Jefferson Co PH
Donna Haugom- Jefferson Co EM
Jim Acker- Watertown Fire
Alison Chouinard- Rock County PH
Asa Rowan- Community Health Systems
Mary Crowley- Juneau Co PH
Mike Lohmeier- SCWIHERC/UW Health
Jeff Ethington- UW Organ and Tissue Donation
Joni Marty- Green Co PH
Tanna McKeon- Green Co EM
Jane Gervais- Adams Co EM
Nathan Bubenzer- Meriter
Erica Kane- EMSC/CHAW
Libby Halma- EMSC/CHAW
Marla Noordhof- Beaver Dam Community Hospital
Doug Voegeli- PH Madison Dane Co
Sharon Warden- Mile Bluff Medical Center
Christal Foreyt- Gunderson Boscobel Hospital and Clinics
Sharon Foley- Divine Savior Healthcare
Angie Cohen- Grant Regional Health Center
Amy Hollis- Monroe Clinic
Jill Lenz- Columbia Co PH
Tracy Buchman- Stoughton Hospital
Tina Strandlie- Stoughton Hospital
Dave Larson- Madison VA
Cassidy Walsh- Sauk Co PH
Joe Meagher- Dodge Co EM
Jennifer Justus- Mercy Walworth
Mandy McGowan- UnityPoint at Home
Karen Sell- Columbus Community Hospital
Juan Cullum- Mercyhealth Janesville
Stephanie Kuschel- NIPARC
Ron Krause- Mercyhealth
Kyle Schaefer- UW Hospital
Mike Stephens- UW Hospital
Steve Haskell- UW Hospital
Ben EIthun- UW Health AFCH
Barb Kuska- Beloit Health System
Lynda Brereton St. Mary’s Madison
Stephanie Lehmann- SSM Health
Bob Swenarski- St. Mary’s Janesville
Jon Erdmann- Divine Savior Healthcare
Tom Eliison- UW Health
Dan Williams- SCRTAC
Bill Brotzman- Badger Prairie Healthcare Center
Kim Cox- WI DHS OPEHC
Svea Erlandson- WI DHS OPEHC
Online:
Alice Salli- Mendota Mental Health
Allison Davey- Marquette Co PH
Bill Ritzer- Reedsburg Area Medical Center
Brian Allen- Southwest Health
Carmen Luther- Reedsburg Area Medical Center
Elisa Stott- Beaver Dam CH, Beloit MH, Edgerton HHS
Lisa Pickarts- Sauk Prairie Hospital
Sally Blackbourn- Memorial Hospital of Lafayette County
Samantha Marcelain- Gundersen Moundview Hospital
Sharon Rateike- St. Mary’s Janesville
Suzanne Schreiner- Adams Co PH
Sean Marquis- Mercyhealth
SCWIHERC Family Assistance Center Workshop
Click here for resources