Author: schcc
SCWIHERC Power Outage Exercise May 15, 2024
SCWIHERC will be conducting a Functional Exercise on the scenario of a widespread community power outage caused by severe warm weather on May 15, 2024 from 9AM-Noon. The location where this event will be hosted varies based on the county with which the participant wants to play. Once registered, each participant will receive information about their exercise location closer to May 15.
The target participants for this exercise include public health, hospitals, clinics, long-term care, home health agencies, dialysis providers, emergency management, EMS, fire, law enforcement, power companies, and others that have a role in responding to power outage emergencies at the local level. Please help us spread the word about this exercise to these sectors!
Registration for this exercise is available here: 2024 SCWIHERC Exercise Registration – May 15, 2024
***Note that Sauk County will not being participating on May 15 due to a scheduling conflict. A different date for the exercise is being determined and will be shared with Sauk County partners when available.***
Themes of this exercise include:
- How public safety and healthcare organizations are going to gather information and assess impacts of the power outage.
- How all partners are going to plan and conduct outreach and coordinate response in the community, with respect to prioritizing life safety and health equity for those with functional and access needs and at-risk populations.
- How all partners are going to ensure the continuity of healthcare and public safety service delivery within their own organizations, with respect to assessing impacts, coordinating response, and planning for recovery. These discussions should cover business operations, facility impacts, and staff and other resource management.
- How healthcare partners are going to respond to surge resulting from the decompensation of individuals in the community as a result of the power outage and any lingering impacts of the weather.
- How jurisdictions can request and utilize Health and Human Services EmPOWER data to inform their decision making, including a module wherein a mock EmPOWER data set will be provided, and partners can explore how to use it collaboratively to support information gathering and sharing, and response coordination.
February 6, 2024 Membership Meeting
SCWIHERC February 6, 2024 Membership Meeting Notes
Meeting Recording:
Passcode: see email from Jennifer February 7.
Hospital:
Dave Larson (Madison VA) recapped a recent internal flood event. Lessons learned: do frontline staff know who the correct person to contact in an emergency (is this easily found in the emergency response guide?) It is important to assess the situation yourself to verify incident and inform response (just how big and impactful is the flood?) Can you repurpose unoccupied clinical spaces to move a unit rather than evacuating or going on diversion? Think about this ahead of time.
Review ASPR TRACIE Utility Failures in Healthcare Toolkit: https://files.asprtracie.hhs.gov/documents/utility-failures-in-health-care-toolkit-summary.pdf
Match Survey: Every year, we ask you to report any exercises sponsored by your facility and any significant real events affecting your facility that resulted in the activation of your EOP to our Match survey. ASPR requires that Wisconsin HERCs match10% of our grant funding award every year, and we do this by capturing in-kind efforts in the form of preparedness and response work you do within your own facility, so thank you for your assistance with this! Survey link: https://www.surveygizmo.com/s3/3321278/WHEPP-Exercise-and-Real-Event-Report-F-02007-06-2022
MRSE Prep: Final deadline for hospitals to register is Monday, February 12, to allow facilitator to create paper patient profiles for each participating hospital. There will be injects related to family reunification again this year, think about using EMTrack to help with this function. If you want to use EMTrack, please review this video, and reach out to me a week ahead of time to ensure EMTrack user access, and if you need dummy tracking numbers (rather than using your own triage tags). Video: https://youtu.be/LOFIUfGBwAA
Discussion question: Why are hospitals (inpatient units and EDs) so full right now? Hard to discharge to post-acute care impacting throughput/causing backups all the way to the ED, staffing impacting how many units can be open to patients, respiratory season, hard to transfer to higher level of care/psych, Medicaid unwinding impacting primary care availability, also leading to decompensation and increased ED traffic, silver tsunami (Baby Boomer retirements combined with increased need for care). Is this our new normal post-COVID? COVID exposed fragility of healthcare system. Highlighting lack of viable solutions to these problems without systemic changes to policy and reimbursement, which leads us to…
Northwest Wisconsin closure of two hospitals (Sacred Heart Eau Claire and St. Joe’s Chippewa Valley) and 19 clinics. This closure closes a level III trauma center, and will leave two hospitals in Eau Claire. EMResource data from last year shows all three Eau Claire hospitals spending more than half of the time at peak census for hospital census. Also impacts rehab hospital, adult and child psych, referral lab and imaging svcs, home care and hospice, numerous other services. Already seeing major impacts in that healthcare market and beyond, because some services already ceasing even though final closure date is April. Related media articles:
https://www.weau.com/2024/01/30/data-reveals-financial-situations-chippewa-valley-hospitals/
https://www.weau.com/2024/01/30/reimbursement-challenges-wisconsin-hospitals/
Next Hospital Forum March 20 at noon.
Membership:
HVA Survey due February 21.
Nurses Respond Now course and scholarships still available, see email from Jennifer on January 4.
We are approaching budgeted limit for SCWIHERC scholarships, submit soon if you wish to be considered. See email from Jennifer on November 3.
UW Health has resources to support Stop the Bleed training, you can borrow equipment and provide your own instructors, or request their instructors. See attached flyer.
Upcoming Trainings: review email from Jennifer February 1, BDLS/ADLS in 4 weeks! We have three seats remaining for our region, reach out to Jennifer to register. WI DHS will also be hosting an EMResource and EMTrack live training on February 13 at noon, this is a great opportunity for a refresher or to train new staff. Register here: https://events.gcc.teams.microsoft.com/event/1ba3b6f4-f488-4c6d-83f3-d88c014f7a46@f4e2d11c-fae4-453b-b6c0-2964663779aa
Cybersecurity Workshop- one offering April 23-24 in Oshkosh, and another offering pending venue confirmation, likely Menomonie in June. This offering is heavily tailored to healthcare, but we can accommodate local government that supports public health, EM, EMS if they can send the required team. To be eligible to register, an organization will have to commit to sending a team of four on the first day (TTX) to include IT/cyber lead(s), operational leader, emergency manager/business continuity plan writer, and one ancillary services rep. Team of two needed for second day (business continuity plan development), to include operational leader and emergency manager/business continuity plan writer. Organizations are strongly encouraged to designate backups for their teams to fully leverage this opportunity, in case unforeseen emergencies prevent a team member from attending.. To be equitable, registration will be limited to one per healthcare system. Official registration email will be shared when venue contract is confirmed for second workshop. Our region has 6 organization slots for Oshkosh offering, and 3 organization slots for Menomonie offering.
Exercises update:
Medical Response and Surge Exercise on February 27, hospitals please invite your local PH/EM/EMS into your command center to strengthen local relationships and work through collaborative injects in the exercise! Registration link for exercise participants (hospitals also need to respond separately if they are playing to receive paper patients): https://zoom.us/meeting/register/tJIqduiupz8tE9c1lysrgNc0eargHbMnTh1-#/registration
Chemical Surge Annex plan review and related TTX will be the topic of May 7 SCWIHERC meeting. In person and virtual options will be provided.
Update to Power Outage exercise: initially we had planned to offer this as a tabletop exercise with one really large group, but the staffing cost to support this is cost-prohibitive. We are now asking county Emergency Managers to host locally, and connect to virtual facilitation, so participants still have the benefit of local networking and collaboration in person with fellow local responders, and we can still offer this exercise within our budget. This offering is not a grant requirement, but a high priority for us with power outage ranking #2 on our regional HVA. Utilizing carryover funding opportunity to bring this to you because it is too costly for our current base budget, and that carryover funding expires June 30. We are reviewing proposals and will get an exercise save the date out as soon as a facilitator is selected.
Speakers:
Strategic National Stockpile and Chempack:
Kay Mittelstadt-Lock and Curtis Hedman, WI DHS Kay.mittelstadtlock@dhs.wisconsin.gov Curtis.Hedman@dhs.wisconsin.gov
Slides are attached. Also refer to this guidance on Fourth Generation Agents:
https://chemm.hhs.gov/nerveagents/FGA.htm
https://chemm.hhs.gov/nerveagents/FGA_Safety_Awareness_Bulletin_508.pdf
https://chemm.hhs.gov/nerveagents/FGA_Reference_Guide_508.pdf
https://chemm.hhs.gov/nerveagents/FGA_Medical_Management_Guidelines_508.pdf
Republican National Convention Update:
Michelle McKinney michelle.mckinney@dhs.wisconsin.gov
RNC Hospital Checklist should be available very soon and will be shared at that time, will be discussed at future SCWIHERC Hospital Forums. Our region should anticipate impacts from RNC activities!
ATT FirstNet Update:
Aaron Midthun Aaron.Midthun@ATT.com 715-559-9057
Refer to meeting recording for full details from speakers.
Sharing resources from the National Healthcare Coalition Preparedness Conference, which four SCWIHERC reps attended:
HIGHLY recommend Miami Dade LE Active Shooter video (12 minutes), to engage your leadership and local law enforcement on the threat of active threat inside a healthcare facility!
Pediatric Readiness:
https://www.chawisconsin.org/initiatives/emergency-care/emergency-department-readiness/
https://www.chawisconsin.org/initiatives/emergency-care/pre-hospital-readiness/
https://wrap-em.org/index.php/jit-resources/pediatric-surge-playbook
https://www.npdcoalition.org/resources/
https://pedspandemicnetwork.org/
ASPR TRACIE Utility Failures in Healthcare Toolkit: https://files.asprtracie.hhs.gov/documents/utility-failures-in-health-care-toolkit-summary.pdf
Get to know your NWS Warning Coordination Meteorologist and get on their weather alert distro list: NWS Milwaukee: timothy.j.halbach@noaa.gov
PsySTART: https://www4.psystart.net/
Miami Dade LE Active Shooter in Hospitals video: https://www.mdchpc.org/resources.html
Pathways to Health Equity: https://webassets.nationalacademies.org/healthequity/
Meeting attendance:
Marcus Walden- MMC Beaver Dam
Nathan Bubenzer- Meriter UPH
Sarah Jensen- Marquette County HD
Jane Lentz-Gervais- Adams County EM
Dave Kitkowski- St. Clare Baraboo and SCWIHERC
Alaina Landerud- St. Mary’s Madison
Belle Koch- Sauk Prairie Healthcare
Angie Cohen- Grant Regional Health Center
Jim Abitz- Southwest Health Platteville
Jeff Kindrai- Grant County HD
Anthony Rauterberg- Watertown FD
Mile Bluff Medical Center
Brent Skiba- Watertown RMC
Dan Perdue- SSM Health
Gary Trulson- UW Health
Mary Tessendorf- Monroe Hospital
Sam LaMuro- Fort HealthCare
Mike Stephens- Fort HealthCare and SCWIHERC
Colleen Wilson- Waupun Memorial
Dave Larson- Madison VA
Steve Haskell- UW Health
Tammy Kingery- Gundersen Moundview
Leanne Seifert- Watertown RMC
Carmen Luther- Reedsburg AMC and SCWIHERC
Sean Madison- NIPARC
Lori Mertens Pelliteri- Dean Clinics
Keith Hurlbert- Upland Hills Health
Christal Foreyt- Gundersen Boscobel
Jodi Moyer- Beloit Health System
Brian Allen- Southwest Health Platteville
Brooke Fuchs- Rainbow Hospice
Lynn Skatrud- Green County HD
Cody Kowalke- Reedsburg AMC
Carmen Carpenter- Iowa County HD
Gary Ziegler- Green County HD
Jodie Molitor- Sauk County HD
Ken Van Horn- PH Madison and Dane County
Jessie Phalen- Sauk County HD
Josh Kowalke- Reedsburg Ambulance and SCWIHERC
Victoria Parker- Watertown HD
Kimberley Spurgeon- Family Health La Clinica
Michael Niles- Rock County HD
Erin Hastert- Lafayette County HD
Kara Takes- Unified Therapy
Michelle Sullivan- Unified Therapy
Mike Lohmeier- SCWIHERC and UW Health
Kay Mittelstadt-Lock- WI DHS
Curtis Hedman- WI DHS
Jason Witte-WI DHS
Michelle McKinney-WI DHS
Hannah Segaloff- WI DHS
Aaron Midthun- ATT FirstNet
Jennifer Behnke-SCWIHERC
November 14, 2023 Membership Meeting
Agenda:
SCWIHERC November 14, 2023 Membership Meeting Notes
Meeting recording: https://us06web.zoom.us/rec/share/LdGrskDvUDukdvjAw55DwJDpqYYfXUGytCwHM3f4DnewaxU7ygSc85xmp6TuWCC2.CzBqgIcoEGIn7bc4n
Passcode: see email from Jennifer November 16
Hospital
The hospital group discussed the warehouse survey and discussed the balance of adequate inventory versus space available. The DASH Tool https://dashtool.org/ is robust and a bit overwhelming, and likely a starting point. Note that the DASH Tool does let you export results after entering your data.
Suggested meeting topic: FirstNet communications capabilities. Will work to bring this topic in for a future meeting.
The Hospital Forum will skip meeting in December, Jennifer will send out a survey to schedule for early January.
Membership
Jennifer gave a few SCWIHERC updates. The Training Needs Assessment Survey was sent out October 25 and will close November 24. This is very important and our primary source of information for planning trainings in the region and state, please strive to have at least one response per organization, but multiple people from the same organization are welcome to respond! The ventilator survey, sent Nov 8 and Due Nov 20, can be used to request no-cost ventilators from WI DHS stockpile. SCWIHERC applied for carryover funding to support a cybersecurity workshop and conduct a power outage tabletop exercise. Cyber is #3 on our HVA, and WICTRA https://wictra.org/ hosts a two day workshop wherein the first day is doing a TTX to discover your organizational vulnerabilities, and the second day is used to write a cyber event continuity plan. Power Outage is # 2 on our HVA, and we are looking to host an in-person tabletop exercise like the good old days where we would be grouped together with our local response partners, and cover response to a substantial power outage which affects health partners but also impacts the community. Other smaller projects for which SCWIHERC requested carryover money include refreshing our website, and continuing our fundraising efforts as a nonprofit organization. Don’t forget that SCWIHERC is offering scholarships to support emergency preparedness efforts in the region, see email sent November 3. Also note the following scheduled spring dates: Feb 6 and May 7 for SCWIHERC meetings, February 21 for Medical Surge and Response Exercise (MRSE).
Jim Oleson, WI DHS Warehouse Supervisor, gave an update on warehouse operations. The state has a glut of supplies received during the pandemic, and needs to demobilize and return to pre-pandemic operations and par levels. This is the reason behind the warehouse survey which closed yesterday, November 13. Refer to recording for more details, questions can be sent to james.oleson@dhs.wisconsin.gov
Ann Zenk, Wisconsin Hospital Association, gave a presentation on workforce development and WHA’s work on this topic to train and retain the healthcare workforce. azenk@wha.org
Traci Lindsey, South Central Wisconsin Area Health Education Centers, also gave a presentation describing SCWAHEC’s mission and work on this topic. They are interested in hearing from you if your organization can take interns or mentor students in some capacity! trlindsey@scwahec.org
Refer to the recording for more details.
What are we working on and preparing for?
MCI preparedness, upcoming respiratory season, staffing shortages/hiring/retention, cyber threats, decon, PHEP and other emergency plan updates.
Meeting attendance:
Jeff Brown- Mercyhealth
Dave Kitkowski- St. Clare Baraboo and SCWIHERC
Michael Niles- Rock County HD
Karen Nsiah-Ababio- Rock County HD
Jordon Denfeld and Derrick- Maxim Staffing
Karmen Bryer- Beloit Health System
Nathan Bubenzer- Meriter UPH
Dave Larson- Madison VA
Belle Koch- Sauk Prairie Healthcare
Mary Crowley- Juneau County HD
Steve Haskell- UW Health
Patti Miller- City of Beloit EM
Angie Cohen- Grant Regional
Jodi Moyer- Beloit Health System
Carmen Luther- Reedsburg Area Med Ctr
Ben Thompson- Mercyhealth
Christal Foreyt- Gundersen Boscobel
Mary Tessendorf- Monroe Hospital
Tammy Kingery- Gundersen Moundview
Adam Dahle- Encompass Health Rehab Hospital
Mike Stephens- Fort HealthCare
Leanne Seifert- Watertown Regional Med Ctr
Sally Blackbourn- Memorial Hospital of Lafayette County
Sharon Rateike- ECRI
Page Heinke- SSM Health at Home
Kyle Schaeffer- UW Health
Emily Kosterman- Waupun Memorial
Katie Budack- Grant Regional
Tina Strandlie- Stoughton Health
Sarah Jensen- Marquette Co HD
Debbie Siegenthaler- Iowa Co HD
Sean Madison- NIPARC
Victoria Parker- Watertown HD
Lynn Skatrud- Green Co HD
Jodie Molitor- Sauk Co HD
Erin Hastert- Lafayette Co HD
Kara Takes- Unified Therapy
Kimberley Spurgeon- Family Health La Clinica
Gary Ziegler- Green Co EM
Anthony Rauterberg- Watertown FD
Diana Quinn- SSM Health
Jeff Ethington- UW Health OPO
Jim Oleson- WI DHS
Ann Zenk- WHA
Traci Lindsey- SCWAHEC
Jennifer Behnke- SCWIHERC
September 19, 2023 Membership Meeting
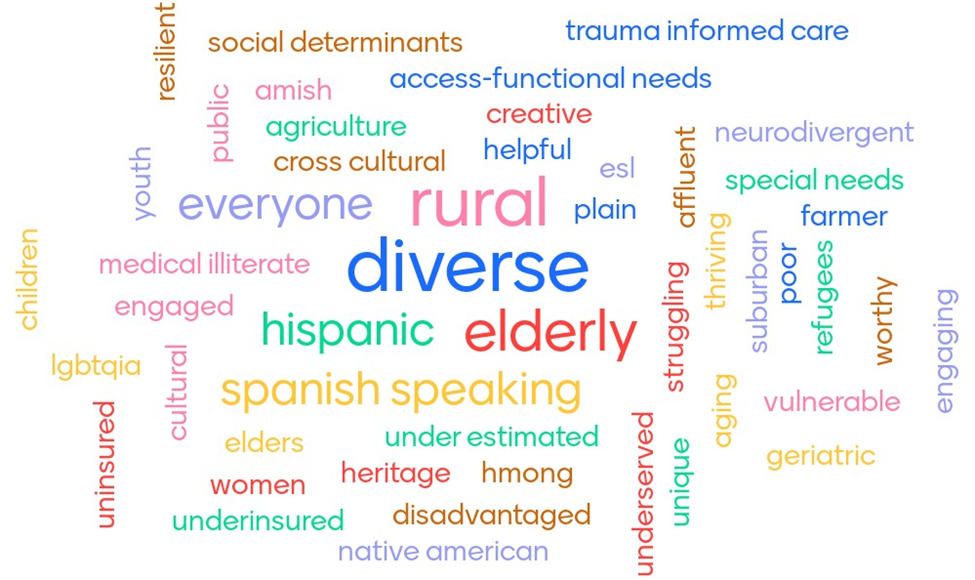
How would you describe the communities we serve?
SCWIHERC 9-19-23 Meeting Notes
Recording:
Passcode: see email from Jennifer on September 21
Hospital:
-Belle Koch of Sauk Prairie Healthcare gave an overview of a recent incident where a 2” water pipe burst and flooded their OB unit and seeped into several other areas, refer to recording for details.
-Mike Stephens of Fort HealthCare gave an overview of a recent event where severe weather resulted in a power outage causing the hospital to run on generator power for over 3 days including one of the chillers. Refer to recording for details.
-These events prompted a discussion on eICS (electronic ICS platform) and how hospitals use mass notification software (emergency notifications vs open clinical shifts), and who receives those.
-All HERCs have access to eICS and use it at a regional level to document response. All partners have the ability to link into SCWIHERC’s eICS for two-way information sharing. Follow up note: there is no discount for eICS through SCWIHERC.
-We held our hospital representative election after reviewing the nominations and bios of two candidates. Mike Stephens of Fort HealthCare was elected as the new hospital rep.
-Next hospital forum meeting is October 19 at noon, where we will do an overview and demonstration of RMCC operations.
Membership:
SCWIHERC Updates: This year’s specialty annex theme is chemical hazards surge. SCWIHERC will be drafting a specialty surge annex on chemical hazards, and then we will conduct a TTX on this hazard at our May meeting. Additionally, we have a grant requirement of conducting a TTX on our Crisis Standards of Care Concept of Operations, which will be integrated into the chem surge tabletop. We will also be facilitating another Medical Response and Surge Exercise.
SCWIHERC Leadership is also working with other HERCs statewide on strategies to support long-term sustainability of the HERCs, and will periodically update at future SCWIHERC meetings.
Some recent updates with our Board of Directors: Aurielle Smith was re-elected to serve as Chair, Dave Kitkowski was elected to serve as Vice Chair, and Mike Stephens was elected as the new hospital representative at this meeting.
We reviewed a presentation and several resources related to whole community planning. The group came up with the word cloud featured above to describe the communities we serve.
The resources mentioned in this presentation are listed here, please note the addition of the CDC Places resource since the agenda was shared. Refer to the recording for the discussion and slides.
Whole Community Planning Resource Links:
- ACEP PLANNING CONSIDERATIONS FOR PERSONS WITH ACCESS AND FUNCTIONAL NEEDS IN A DISASTER: https://www.acep.org/siteassets/sites/acep/media/disaster-medicine/planning-for-persons-with-functional-needs-in-a-disaster.pdf
- ASPR Presentation Reviewing NACCHO Capacity-Building Toolkit: https://www.eventscribe.com/uploads/eventScribe/PDFs/2019/6206/895787.pdf
- CDC Access and Functional Needs Toolkit: https://www.cdc.gov/orr/readiness/00_docs/CDC_Access_and_Functional_Needs_Toolkit_March2021.pdf
- CDC/ATSDR Social Vulnerability Index: https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
- CDC PLACES: Local Data for Better Health: https://www.cdc.gov/places/index.html
- CMIST Framework: https://www.phe.gov/emergency/events/COVID19/atrisk/discharge-planning/Pages/CMIST-framework.aspx
- CMIST Update: https://disasterstrategies.org/blog-post/defining-functional-needs-updating-cmist-by-june-isaacson-kailes-disability-policy-consultant/
- FEMA Inclusion, Diversity, Equity, and Accessibility in Exercises Considerations and Best Practices: https://preptoolkit.fema.gov/documents/d/hseep-resources/idea_guide_final?download=true
- FEMA National Risk Index: https://hazards.fema.gov/nri/
- NACCHO Capacity-Building Toolkit for including Aging & Disability Networks in Emergency Planning: https://www.naccho.org/uploads/downloadable-resources/NACCHO_Aging-and-Functional-Needs-Planning-FINAL.pdf
- Prepared4ALL: https://nationalcenterdph.org/our-focus-areas/emergency-preparedness/prepared4all/online-training/
- Prepared Caregivers: https://www.caregiver.va.gov/support/docs/Prepared_Military_Caregivers_Disaster_Relief_Toolkit_Final.pdf
- Public Health is for Everyone: https://www.phetoolkit.org/
Sharing lessons learned and best practices:
Rock County Health Department has been working on a tool to make better informed decisions on where to set up Points of Dispensing sites, they will keep us posted and also submitted an abstract for the NACCHO Preparedness Summit.
We talked a bit about Air Quality issues over the summer, especially on communications and messaging with the public. Strategized on sharing these messages through other leaders and offices so that the message wasn’t coming from public health, where we feel like there is messaging fatigue post-COVID.
Public Health Madison and Dane County shared their lessons learned from responding to this hazard.
Refer to recording for more details.
Next meeting will be November 14, 1-4PM
Meeting attendance:
Mike Stephens- Fort HealthCare
Lisa Herritz- Ho-Chunk Nation
Christal Foreyt- Gundersen Boscobel
Victoria Parker- Watertown HD
Michael Niles- Rock County HD
Karen Nsiah-Ababio- Rock County HD
Tom Ellison- UW Health
Nathan Bubenzer- UPH Meriter
Tina Strandlie- Stoughton Health
Dave Kitkowski- St. Clare Baraboo and SCWIHERC
Tammy Kingery- Gundersen Moundview
Carmen Mihlbauer-Luther- Reedsburg AMC
Ben Thompson- Mercyhealth
Emily Kosterman- Waupun Memorial
Angie Cohen- Grant Regional
Geana Shemak- Iowa Co HD
Ian Fisher- Marshfield Health System
Ken Van Horn- PH Madison and Dane County
Belle Koch- Sauk Prairie Healthcare
Steve Haskell- UW Health
Ed Somers- Clearview
Erin Hastert- Lafayette Co HD
Sally Blackborn- Memorial Hospital of Lafayette Co
Mike Hall- SSM Health Monroe/Janesville
Haley Schreiber- St. Mary’s Janesville
Mary Tessendorf- Monroe Hospital
Jason Witte- WI DHS EMS
Jeff Ethington- UW Health OPO
Brooke Fuchs- Rainbow Hospice
Kara Takes- Unified Therapy
Jessie Phalen- Sauk Co HD
Lynn Skatrud- Green Co HD
Paige Heinke- SSM Health Home Care
Sean Madison- NIPARC
Jodie Molitor- Sauk Co HD
Darienne Blair- Columbia Co HD
Carrie Meier- Dane Co EM
Aurielle Smith- PH Madison and Dane Co, SCWIHERC
Leanne Seifert- Watertown RMC
Taylor Fish- Sauk Co PH
Kelly Heysinger- Unified Therapy
Jennifer Behnke- SCWIHERC
May 17, 2023 Membership Meeting
May 17, 2023 Membership Agenda
Recording link and passcode: See email from Jennifer on May 20.
Hospital:
We discussed how hospitals should prepare for the Medical Response and Surge Exercise on June 14. The scenario will give each hospital a 20% surge of paper patients based on the bed survey responses. The premise of the exercise is that hospitals will then look at their real census and staffing on exercise day, and move through their paper patient surge to determine how many patients they can make room for, how many current admissions where they can expedite discharge, and whether they have enough supplies to care for the paper patients in this scenario. Please consider inviting your local EMS, interfacility transport, public health department, and emergency management reps to your hospital command center during the exercise. There will be a hotwash immediately after the conclusion of the exercise, and we will also talk more in-depth at our June Hospital Forum meeting (June 20 at noon) about how hospitals responded and overall themes, strengths, and areas for improvement.
Reminder that hospitals are asked to complete the MATCH survey to report their in-kind efforts on exercises and real events. These survey responses help the Hospital Preparedness Program meet our 10% grant matching requirement from the feds. Deadline for survey completion for this grant year is June 30 (we will ask again for activities starting July 1 next year). MATCH survey link: https://www.surveygizmo.com/s3/3321278/WHEPP-Exercise-and-Real-Event-Report-F-02007-06-2022
ABLS continues to be a hassle, without warning we learned ABA changed learning platforms about 6 weeks ago, current course progress was lost if the course wasn’t finished at that time, and users cannot find where to access the course on the new platform. Jennifer sent out an email on May 8 to all users on her master registration list requesting that they attempt to log in and find the course, and if it is not there, to reach out to ABLS (ABLS@ameriburn.org) to put in a support ticket. Users should do this before they attempt to resume the course, to be sure the course is actually there when they need it! Related to the Burn Surge Plan- don’t forget to share/post the burn plan activation one-pager so your staff know when and how to activate the burn plan. Link:
We reviewed the poorer than usual EMResource response rates, especially to mass casualty incident type events. Typically two root causes: training is needed to show staff how to do it correctly, or alerts are not getting to the staff tasked with responding. Remember that notification methods include text message (to personal or pass around phones), email, and voice alerts (robodial that can also go to a landline). Group expressed an interest in continued reminders to keep addressing the problem, Jennifer will also compile response rates and share soon. Remember that the success of the RMCC, and more importantly better patient outcomes, are supported when hospitals respond. This is the only way for the field to understand your current capabilities based on your current staffing and patient loads!
Membership:
Medical Response and Surge Exercise: Two specific injects written into exercise to engage local public health and emergency management. Please join your hospital command center in person so you can learn from each other and learn what you can offer each other in this scenario. Even if you cannot be there in person, your hospitals (or the exercise controllers) will reach out to you during the exercise for support on these injects. Please discuss with your staff how you would respond to these injects and add that to feedback survey or email to Jennifer.
SCWIHERC will be doing annual review of plans, making updates, and requesting documentation that your organization received our plans via DocuSign in Junem completion requested by June 30. This is an annual federal requirement that HERCs must meet to show the feds that we pr ovided these plans to our partners, your completion of the DocuSign is our official documentation for this requirement.
Several opportunities remain from now until June 30: Flyers for all are attached.
Media Relations Workshop June 1, 11 seats remain
Active Shooter Incident Management Basic for First Responders June 6 or 7, 60 seats remain
CMS Virtual Exercise June 21, room for 100 more organizations! Please continue to target and share this with long-term care facilities, hospices, home health agencies, ambulatory surgery centers, outpatient physical/occupational therapy providers, end stage renal disease (dialysis) providers, federally qualified health centers, rural health centers, and intermediate care facilities for individuals with intellectual disabilities. This exercise is customized to these audiences to help test their emergency operations plan, communication plan, and help them satisfy an exercise requirement!
Mark Paulson, WI DHS Radiation Protection Section Manager, joined us to give a presentation on their office and the support and resources offered. Refer to recording and remember that these resources can be reached 24/7 at 608-258-0099 (WI DHS emergency line).
We then proceeded through the tabletop exercise on a radiation injury scenario (SitMan link: ). This is here for your organization if you would like to review this scenario internally with your staff and leadership. https://drive.google.com/file/d/1W4BTeB51-XwBKA8e6L2PPiSjJ7tyoqjg/view?usp=share_link
Other helpful resources:
Radiation Emergency Assistance Center/Training Site: https://orise.orau.gov/reacts/index.html
WI DHS web page that links to a lot of the resources below and some WI specific guides: https://www.dhs.wisconsin.gov/radiation/protection/index.htm
Radiological Dispersal Device (RDD) Response Guidance Planning for the First 100 Minutes: Video and link to guidance https://www.dhs.gov/publication/st-frg-rdd-response-guidance-planning-first-100-minutes
First 100 minute guidance https://www.dhs.gov/sites/default/files/publications/nustl_rdd-responseplanningguidance-public_28oct2021-508-revised.pdf
CDC Population Monitoring and Reception Centers: https://www.cdc.gov/nceh/radiation/emergencies/populationmonitoring.htm?msclkid=79e6b5b7d14411ec9ad290c77bf9f899
Guide to operating shelter during a radiation emergency: https://www.emergency.cdc.gov/radiation/pdf/operating-public-shelters.pdf
Points of Dispensing to Community Rection center planning toolkit: https://www.cdc.gov/nceh/radiation/emergencies/pdf/POD_to_CRC_Planning_Tool-508.pdf
Video and job aid for screening people for external contamination: https://www.cdc.gov/nceh/radiation/emergencies/screeningvideos/index.htm
Just in time training resources and quick reference guides for clinical staff: https://orise.orau.gov/resources/reacts/references.html
Radiation Injury Treatment Network: https://ritn.net/
ASPR TRACIE: https://asprtracie.hhs.gov/technical-resources/32/radiological-and-nuclear/27
Some strengths and areas of improvement from our discussion will be captured and shared in a brief after action report and improvement plan in the next few weeks.
Next meeting in new grant year yet to be scheduled, but likely in September, watch email!
Meeting attendance:
Lisa Herritz- Ho Chunk Nation
Jim Abitz- Southwest Health
Angie Cohen- Grant Regional
Steve Haskell- UW Health
Belle Koch- Sauk Prairie
Jodi Moyer- Beloit Health System
Matt Christian- Marshfield Medical Center Beaver Dam
Nathan Bubenzer- Meriter UPH
Lyle Kratochwill- Richland Hospital
Carmen Luther- Reedsburg AMC
Diana Quinn- SSM Health
Chad Atkinson- Mercyhealth
Christal Foreyt- Gundersen Boscobel
Dave Larson- Madison VA
Paige Heinke- SSM Health
Colleen Wilson- Waupun Memorial
Mike Hall- Monroe Hospital
Carol Quest- Watertown PH
Eric Anderson- Dane County EM/EMS
Dave Kitkowski- St. Clare Baraboo
Joe Meagher- Dodge County EM
Sharon Rateike- St. Mary’s Janesville
Lisa Peters- Gundersen Moundview
Tom Ellison- UW Health
Tammy Kingery- Gundersen Moundview
Leanne Seifert- Watertown RMC
Carmen Carpenter- Iowa County PH
Brent Skiba- Watertown RMC
Mike Stephens- Fort Health Care
Loni Hefner- Access Community Health Centes
Samroz Jakvani- Jefferson County PH
Hannah Sedlacek- Adams County HHS
Victoria Parker- Watertown PH
Matt Bartol- Dodge County EM/PH
Erin Hastert- Lafayette County PH
Kimberley Spurgeon- Family La Clinica
Lynn Skatrud- Green County PH
Michael Niles- Rock County PH
Jeff Kindrai- Grant County PH
Stacy Blakemore- Sauk Co EM
Gary Ziegler- Green County EM
Josh Kowalke- Reedsburg Area Ambulance
Roman Mullen- Dodge County PH
Carol Brown- Rainbow Hospice
Lisa Schweitzer- SSM Health
Sarah Jensen- Marquette County PH
Mark Paulson- WI DHS
Aurielle Smith- Public Health Madison and Dane County, SCWIHERC
Mike Lohmeier- SCWIHERC and UW Health
Dan Williams- SCRTAC
Jennifer Behnke- SCWIHERC
March 22, 2023 Membership Meeting
SCWIHERC 3-22-23 Meeting Notes
Recording: See email from Jennifer on March 24 for link and passcode.
Hospital:
We discussed the end of the Public Health Emergency and how the hospitals are modifying policies in response. There is quite a bit of variability in policies regarding masking for patients, visitors, clinical and non-clinical staff. This is an evolving topic and those still requiring masking continue to discuss and prepare for changing those policies soon.
We discussed the DASH Tool and many had an opportunity to use it since our last meeting. Consensus is that the tool is straightforward and easy to use. https://dashtool.org/ Related webinar: https://files.asprtracie.hhs.gov/documents/aspr-tracie-disaster-available-supplies-in-hospitals-dash-webinar-ppt.pdf Many noted that their current inventory management systems also account for certain scenarios and increased burn rates that are also considered by the DASH Tool.
Next Hospital Forum is April 12 at noon, will resume discussion on TJC New Emergency Management Standards that was started in February.
Membership:
SCWIHERC is planning several activities before June 30:
| Activity | Target Audience | Notes | Proposed Date(s) |
| Radiation Injury Annex Review and TTX | Everyone | Next Regional Meeting | May 17- scheduled! |
| Medical Response and Surge Exercise (MRSE) | Hospitals, everyone | Virtual functional, about three hours | June |
| CMS Partners Virtual Exercise | SNF, Home Health, Hospice, Amb Surgery Ctrs, ESRD providers, PT/OT, FQHC, RHC, ICFIID | Virtual functional, about three hours | June |
| Media Relations Workshop | Partners who deal with the media | In-person workshop, 6-8 hours | June |
| Active Shooter Incident Management Basic (with TtT) | First Responders | Students: 4 hour slots over two days Trainers: both full days | June |
| Tech Systems In-service (EMResource, EMTrack, eICS, WEAVR) | Anyone who uses any of these systems and wants to learn more/needs a refresher (new staff!) | Virtual over Zoom, come and go for each session (60-90 min) as you wish | May |
All activities will be promoted by email when the dates are confirmed and registration is available.
Final HVA is available and posted to SCWIHERC shared drive. Of note: supply chain, staffing shortage, and workplace violence have all moved up in ranking, and are recent additions to the HVA.
We had a lengthy discussion on Supply Chain. This is our #7 ranking hazard on our regional HVA. Vulnerabilities exposed or exacerbated by pandemic continue to exist today. This topic is emphasized by HPP grant and ASPR TRACIE because it is so impactful to response to all hazards!
Refer to the discussion questions in separate attachment, and this resource: https://files.asprtracie.hhs.gov/documents/aspr-tracie-partnering-with-the-healthcare-supply-chain-during-disasters.pdf
Organizations are encouraged to facilitate internal discussion on this topic.
Refer to the recording for full discussion, some very high level themes and takeaways:
-Supply chain for both pharmacy and other materials is incredibly complex. We appreciate our materials management partners for everything they do to obtain the supplies we need to care for patients. Maintaining relationships with vendors is critical.
-Pharmacy shortages are not new but possibly more prevalent now. Constant state of reaching out to health system motherships, retain pharmacies, other potential sources. Entire pharmacy roles exist just to modify formularies and communicating changes to clinical staff is constant.
-The task of balancing is constant: just in time delivery and lean principles vs paying and storing a glut of supplies that may never be used. This is a struggle for all orgs.
-Small wholesalers and creative partnerships and resources have been a lifeline in the past: homemade supplies, partnering with others who can produce items we need (face shields, hand sanitizer, 3D printing)
-Suggested systemic measures to improve situation include government incentives for increased production, onshore/domestic production to significantly cut lead and shipping time could relieve allocation pressure.
What are we concerned about right now? ED Boarding, lack of post-acute care discharge beds, lack of transportation for patient transfer, delayed care keeping acute care busy, ED is the primary care of last/only resort so they stay full. Chronic issues!
- Meeting attendance:
- Angie Zastrow- Rainbow Hospice
- Nathan Bubenzer- UPH Meriter
- Chad Atkinson- Mercyhealth
- Belle Koch- Sauk Prairie Healthcare
- Gary Trulson- UW Health
- Jessica Palzewics- Marshfield Medical Center Beaver Dam
- Jodi Moyer- Beloit Health System
- Karmen Bryer- Beloit Health System
- Bob Swenarski- St. Mary’s Janesville and SCWIHERC
- Nikki Ripp- Adams County HHS
- Casey Farnum- UW Health
- Loni Hefner- Access Community Health Centers
- Seaton
- Chris Brownell- Grant Regional Health Center
- Dave Larson- Madison VA
- Lynn Skatrud- Green County HD
- Mary Crowley- Juneau County HD
- Lori Mertens Pelliteri- Dean Clinics
- Christal Foreyt- Gundersen Boscobel
- Jane Lentz-Gervais- Adams Co EM
- Colleen Wilson- Waupun Memorial
- Marie Darling Ellis- Columbia County HHS
- Diana Quinn- SSM Health
- Bill Sobaskie- Madison VA
- Mike Hall- Monroe Hospital
- Leanne Seifert- Watertown Regional Med Ctr
- Lisa Herritz- Ho-Chunk Nation
- Carmen Mihlbauer-Luther- Reedsburg Area Med Ctr and SCWIHERC
- Tina Strandlie- Stoughton Health
- Daniel Pease- Town of Beloit Fire
- Carmen Carpenter- Iowa Co HD
- Eric Anderson- Dane County EM/EMS
- Charlie Johnson- St. Mary’s Madison
- Kimberley Spurgeon- Family Health La Clinica
- Hannah Sedlacek- Adams Co HHS
- Jeff Kindrai- Grant Co HD
- Jason Witte- WI DHS EMS
- Erin Hastert- Lafayette Co HD
- Kara Takes
- Jessie Phalen- Sauk Co HD
- Paige Heinke
- Patti Miller- City of Beloit EM
- Gary Ziegler- Green Co EM
- Matt Bartol- Dodge Co PH/EM
- Michael Niles- Rock Co HD
- Samroz Jakvani- Jefferson Co HD
- Sarah Jensen- Marquette Co HD
- Matt Christian- Marshfield Medical Center Beaver Dam
- Sally Blackbourn- Memorial Hospital of Lafayette Co
- Dan Williams- SCRTAC
- Mike Lohmeier- SCWIHERC and UW Health
- Jennifer Behnke-SCWIHERC
SCWIHERC’s Solicitation Opportunities
SCWIHERC is seeking proposals for facilitation support for a Power Outage TTX. See full RFP for details, proposals due February 14, 2024.
SCWIHERC Power Outage FE RFP spring 2024
SCWIHERC’s Current Solicitation Opportunities
View current postings for doing business with SCWIHERC!
January 25, 2023 Membership Meeting
SCWIHERC 1-25-23 Meeting Notes
Recording: see email from Jennifer on January 26.
Hospital Meeting:
ABLS update: still have seats left, still have hospitals in region that haven’t used their seats. All unused seats that were previously earmarked for a hospital in our region will be given up to the first come, first served pool in the region and state if unclaimed after February 10. Then facilities may request extra seats, and other regions may use them as well. Jennifer will send a separate email on this with a specific breakdown of how many seats remain from initial allocation for each facility.
Burn Plan one page quick reference guide: Identified need for this resource after debriefing from Pulaski bonfire incident, wanted to make a resource available for frontline ED staff to know how to activate the burn plan and where to find more information. Please educate your staff on this resource and post where it will be available to them: (in shared drive)
Med shortages: If a medication shortage has been raised to a level of significance that your EOC/IC within your facility is aware of it, please share with Jennifer to be shared for situational awareness to the region (facility will be de-identified), state, feds. State and feds need significant lead time to act on this info, so earlier is better!
Question on readily available safety references and resources for staff that can be included in newsletters etc? Looking for something that has already been created to minimize recreating the wheel. If you identify any, please share with Jennifer.
Public Health Emergency was extended until April, but how are we getting ready to transition to operations after PHE expires and going back to “new” normal? Please start to discuss with your team and share any checklists or resources you have started in anticipation of this task. Jennifer will also look for resources and discuss with other HERC Coordinators.
Anyone using the DASH Tool? Disaster Available Supplies in Hospitals. https://dashtool.org/ Related webinar: https://files.asprtracie.hhs.gov/documents/aspr-tracie-disaster-available-supplies-in-hospitals-dash-webinar-ppt.pdf Recommend entering your information in these forms to find out what your numbers are to start planning and making the case for carrying this inventory of these supplies. Will revisit with March supply chain meeting to continue discussion.
Will discuss new TJC EM standards at next hospital meeting, please bring your questions and discussion points for the group.
Membership Meeting:
Plug for WEM Governor’s Conference, registration and agenda info: https://wigcot.eventsair.com/2023-wisconsin-governors-conference-on-emergency-management-homeland-security Starts end of February in West Madison/Middleton.
HVA Survey due February 24, see email from Jennifer on January 24 for link.
Exercise update: currently soliciting bids for Medical Response and Surge Exercise (MRSE). Must be completed by June 30, goal of exercise day between May and early June. Exercise info: https://aspr.hhs.gov/HealthCareReadiness/guidance/MRSE/Pages/default.aspx Seeking exercise design team members, please email Jennifer if interested! Also NucRad TTX based on draft surge plan to be held May 17 as part of SCWIHERC meeting. NucRad is topic for this year’s specialty surge.
March 22 meeting will have supply chain integrity theme, please invite your internal and external (vendor) supply chain partners!
Anticipating funding to continue SALT Triage Ribbon and RMCC training project this spring, target audience is EMS providers but we should probably offer at least one more session for hospital audience, only about half participated in May 2022.
SCWIHERC is planning a virtual information sharing systems in-service day in late spring, more hands-on approach for using various systems (EMResource, EMTrack, eICS, others?). More info to come.
Sam Anderson, WI DHS OPEHC Training and Exercise Coordinator Samuel.Anderson@dhs.wisconsin.gov Sam talked about the training needs assessment survey results, statewide results included in email from Jennifer January 25 but regional results will also be compiled later. Looking at optimal and efficient planning with expensive course offerings (CHEC, BDLS, ADLS etc.) in the face of limited funding availability.
Presentations and extensive discussion on using EmPOWER tool, refer to recording. https://empowerprogram.hhs.gov/
Mandi Walsh, Health Preparedness and Response Ops Specialist mandi.walsh@dhs.wisconsin.gov
Ken Van Horn, Emergency Preparedness Coordinator, PHMDC KVanHorn@publichealthmdc.com
ONLY Local Health Officer or their designee can request the data! Recommend pulling practice data set out of PCA Portal and practicing sorting and deleting data to find what you need to take action. Ken will share his notes with LHDs when he has a chance.
While using/requesting the response data, we learned that we can speed up the request and implementation by making sure we knew how exactly we could share the files with only applicable people (easy on most systems, not on ours)and, after scrambling to find some people to help sort data on Dec. 23 right before a holiday, are putting together a list of people who can step in and are comfortable with this data set.
Note that coordination of safety checks should triage patients based on the type of device they are relying on and how emergent it is to life safety (cardiac devices, ventilators). Coordinate with your local EOC and EMS to create your own triage criteria. Pros and cons to using law enforcement officers to conduct safety checks: keeps fire/EMS free for response and other 911, but not all communities feel safe answering the door to law enforcement unannounced. Consider in your response planning!
Other current topics: Feds will not mobilize Tamiflu from SNS until all other local/regional resources have been exhausted. More info in email from Jennifer Friday, January 20. What else are we focusing on? Staff burnout and wellbeing. Remember that “Now What?” modules are available on demand from SCWIHERC shared drive under best practices, resiliency. These are in five units and can be used one at a time at small staff meetings etc.
Next meeting: March 22, 1-4PM.
Meeting attendance:
Jane Lentz-Gervais, Adams Co EM
Josh Kowalke, Reedsburg Area Ambulance Service
Mary Crowley, Juneau Co PH
Lynn Skatrud, Green Co PH
Dave Kitkowski, St. Clare Baraboo,
Gary Ziegler, Green Co EM
Victoria Parker, Watertown PH
Ken Van Horn, PH Madison and Dane Co
Tom Ellison, UW Health
Roman Mullen, Dodge Co PH
Nick Metz, Upland Hills Health
Lori Mertens Pelliteri, Dean Clinics
S Eaton, Community Health Systems
Charlie Johnson, St. Mary’s Madison
Lisa Herritz, Ho Chunk Nation
Colleen Wilson, Waupun Memorial
Marie Ellis, Columbia Co PH
Christal Foreyt, Gundersen Boscobel
Ian Fisher, Marshfield Medical Center Beaver Dam
Carmen Luther, Reedsburg Area Medical Center
LuAnn Reuter, Prairie Ridge Health Columbus,
Chad Atkinson, Mercyhealth Janesville
Mike Stephens, UW Health
Jodi Moyer, Beloit Memorial
Emily Kosterman, Waupun Memorial
Sally Blackbourn, Memorial Hospital of Lafayette County
Sarah Jensen, Marquette Co PH
Steve Haskell, UW Health
Colton Ritchie, PH Madison and Dane Co
Dave Larson, Madison VA
Belle Koch, Sauk Prairie Hospital
Katie Budack, Grant Regional
Jennylynde Packham, UW Health Rehab Hospital
Leanne Seifert, Watertown Regional Medical Center
Kimberley Spurgeon
Carol Brown, Rainbow Hospice
Mike Hall, Monroe Hospital
Nathan Bubenzer, Meriter
Tammy Kingery, Gundersen Moundview
Joe Meagher, Dodge Co EM
Jim Abitz, Southwest Health
Mary B, Jefferson Co HD
Bob Swenarski, St. Mary’s Janesville
Keith Hurlbert, Iowa Co EM
Diana Quinn, SSM Health
Angie Cohen, Grant Regional
Dan Williams, SCRTAC
Aurielle Smith, PH Madison and Dane Co
Jeff Kindrai, Grant Co PH
Carrie Meier, Dane County EM
Samroz Jakvani, Jefferson Co PH
Matt Bartol, Dodge County PH/EM
Madison Dillinger
Jodie Moliter, Sauk Co PH
Annie Fridh, Community Health Systems
Carly Tibbits, Iowa Co PH
Patti Miller
Cara MacKenzie
Karen Greenwald, Dodge Co PH
Alesha Erdenberger
RoAnn Warden, Green Co PH
Mary Tessendorf, Monroe Hospital
Julie Staffin, Mayville EMS
Sam Anderson, WI DHS OPEHC
Mandi Walsh, WI DHS OPEHC
Jennifer Behnke, SCWIHERC
SCWIHERC is recruiting a Sustainability Coordinator
Please see the request for application for more details and how to apply. Applications will be accepted until January 4.
Sustainability Coordinator RFA Dec 2022
November 9, 2022 Membership Meeting
SCWIHERC 11-9-22 Meeting Notes
Recording: https://us06web.zoom.us/rec/share/PQWEweQMuvett1Y6doMZ2uxAiWsRWIxKJ2e-ShmfTi13VDo0zbQRmaUqARLRCylN.FFBdmVxW9rubyYJ7
Passcode: See email sent November 10
Hospital Meeting:
EMResource reminders- PEDs surge bed count, update at least once daily, not going away as long as surge is an issue. PEDS ED Boarders expected to go up
ABLS- next batch expiring in February, sending periodic updates. Seat allocation: 5 nonphysician seats for each level III, IV and unclassified, 12 nonphysician setas for each level I and II. 2 physician seats for each hospital. Reach out at any time to enroll new students, check assignment, with other questions.
Open discussion: violent patients and patient security screening. Barriers to implementation- staffing. Seeing increase in threats from patients/visitors. Not necessarily weapons, but more physical aggression/assault directed at staff. Is incidence increasing, or reporting increasing? Both. Increasing visitors d/t decreasing COVID restrictions is a factor.
De-escalation options: Crisis Prevention Institute Nonviolent Crisis Intervention, MOAB (management of aggressive behavior), increasing posted signage on patient/visitor behavior expectations, higher security presence in facility, DT4EMS, active threat drills at service level. Safety solution in another state: installed hotel safes in trauma bays to store contraband/weapons while the patient was admitted, have security staff move weapon off patient. Some states have quite intensive security screening procedures compared to us. Shared escalation policy- green, yellow, red, full lockdown, policy shared by email November 10.
HCID discussion: need a review of Ebola state ConOps and how ETCs/Regional Treatment Centers are involved, include transportation plan.
Membership Meeting:
Leadership review SCWIHERC and OPEHC: http://www.scwiherc.org/category/who-are-we/ or first tab of Coalition phone book in SCWIHERC shared drive.
Fiscal and Sustainability Update- The HERCs have been presented with a lot of new policies that impact how we do business. Grant funds are only reimbursable after expenses have been incurred, so how do we solve cash flow to pay for vendors and services up front? Historically have had the benefit of having a fiscal agent, but now that we are an incorporated legal entity, this is not allowed anymore. Current coping mechanism is HERC staff have been putting expenses on personal credit, which is not advisable or sustainable. To better explore options, SCWIHERC will be recruiting a Sustainability Coordinator to explore our options for revenue sources and cash flow issues. Sustainability Coordinator Request for Application emailed and posted to scwiherc.org on November 10. SCWIHERC Board welcomes any and all suggestions and ideas on how to cope with these issues. Additional fiscal policies that have been recently updated include a Net 30 days from submission turnaround time on funding disbursement, we cannot spend grant funds on food, any HERC travel is reimbursed at the state rate (previously was federal rate), must use state procurement guidelines for competitive bids, and all HERC expenses must be explicitly approved by the state ahead of time to be reimbursed.
Training, Exercises, SALT Triage and RMCC Project and Training: Training needs assessment was sent out October 26, sent again November 10, due Nov 30. Your input is requested and valued!
Working on request for application to find a contractor to assist with planning and conducting our Medical Response Surge Exercise (MRSE), which replaced the Coalition Surge Test (CST) from the before COVID times. This exercise will also test our pediatric surge plan to satisfy another grant deliverable. Plan to use a Wisconsin Dells peak tourism season scenario for surge. Other planned TTX is for radiological surge, which is the topic of our specialty surge annex this year.
Still continuing with SALT Triage and Regional Medical Coordination Center project and training. Offered 5 first receiver train the trainer sessions in May, about half of hospitals participated. Still hoping to have other hospitals participate, please reach out to plan a regional training or to request triage ribbon kits or replacement ribbons. Youtube training video for hospitals: https://www.youtube.com/watch?v=N7OG8a7vXnE
Also continuing to offer similar training to EMS agencies in the region, also incorporating training on RMCC resource-activation and coordination. Reach out to schedule these sessions!
Will Koehne, WI DHS OPEHC Epidemiologist, gave an interview of Hospital Dashboards on PCA Portal, review recording, email Jennifer or Will William.koehne@dhs.wisconsin.gov for access. Other systems’ discussion deferred at this time.
RSV surge- Please update bed count (green banner) daily! What will be the issues with PEDs surge? Short on pediatric providers and staff for both ED and inpatient. Some have developed some education for nursing and family practice to augment clinical care- partner with your respiratory therapy! Jennifer will forward clinical resources from the National Pediatric Disaster Coalition/AAP to hospitals.
No reports of diesel fuel shortage in the region at this time, but have seen elsewhere in the state. Be sure you have a priority contract with your vendor and please relay any news of shortages to Jennifer and your county emergency manager for situational awareness.
No reports of albuterol shortage in the region at this time, but have seen elsewhere in the state. Reports of etomidate, fentanyl, and racemic EPI shortages.
Doug Hill gave an update on Crisis Standards of Care. Note that Wisconsin Hospital Mutual Aid MOU will be sunsetting and not renewed, due to a lack of interest from hospital leaders and WHA. Refer to recording and this 2010 WHA document he referenced: https://www.wha.org/WisconsinHospitalAssociation/media/WHACommon/EmergencyPrep/HospitalsGuideforMassCasualtyEvents6-2010.pdf
Doug Hill can be reached at djh1967@gmail.com
Meeting attendance:
Matt Bartol- Dodge County HHS, EM
Tom Ellison- UW Health
Lyle Kratochwill- Richland Hospital
Christal Foreyt- Gundersen Boscobel
Mary Crowley- Juneau Co HD
Amanda Diedrich- Juneau Co HD
Sarah Jensen- Marquette Co HD
Jodi Moyer- Beloit Health System
S Eaton
Donna Haugom- Jefferson Co EM
Tina Strandlie- Stoughton
Belle Koch, Sauk Prairie Hospital
Carmen Luther- Reedsburg Area Med Ctr
Jim Abitz- Southwest Health
Ron Krause- Mercyhealth
Matt Christian- Marshfield Med Ctr Beaver Dam
Jennylynde Packham- UW Health Rehab
Dan Williams- SCRTAC
Adrianne Bonow
Eric Anderson- Dane County EM
Dave Larson- Madison VA
Mike Stephens- UW Health
Steve Haskell- UW Health
Nathan Bubenzer- Meriter UPH
Katie Budack- Grant Regional
Dave Kitkowski- St. Clare Baraboo
Sam LaMuro- Fort HealthCare
Jodie Molitor- Sauk Co HD
Nina Gregerson- PH Madison and Dane County
Leanne Siefert- Watertown Regional Med Ctr
Karen Greenwald- Dodge Co HD
Kimberley Spurgeon- Family Health La Clinica
Heather Poker- St. Mary’s Madison
Tammy Kingery- Gundersen Moundview
Samroz Jakvani- Jefferson Co HD
Laura Kane- UW Health
Sally Blackbourn- Memorial Hospital of Lafayette Co
Carrie Meier- Dane Co EM
Sharone Rateike- St. Mary’s Janesville
Elizabeth Chilsen- Jefferson Co HD
Nick Metz- Upland Hills Health
Victoria Parker- Watertown HD
Lynn Skatrud- Green Co HD
Emily Kosterman- Waupun Memorial
Jane Gervais- Adams Co EM
Jeff Kindrai- Grant Co HD
Colton Ritchie- PH Madison and Dane County
Ken Van Horn- PH Madison and Dane County
Tanna McKeon- Green Co EM
Debbie Siegenthaler- Iowa Co HD
Andrea Murleau
Madison Dillinger
Chad Atkinson- Mercyhealth Janesville
Will Koehne- WI DHS OPEHC
Doug Hill- CSC Project
Aurielle Smith- PHMDC and SCWIHERC
Mike Lohmeier- UW Health and SCWIHERC
Jennifer Behnke- SCWIHERC
June 15, 2022 Membership Meeting
June 15 SCWIHERC Membership Meeting Notes
Passcode: See email sent June 15
Reminder that DocuSign signatures for annual plan review are due June 30. Reminder email was sent directly to signer on file for your organization. Will resend any unsigned plans 7-10 days before deadline.
Upcoming Trainings and Information:
| Course | Location | Date | Link if available |
| MGT-341; Dis. Preparedness Hosp/HC | Spooner | October (TEEX still determining exact date) | |
| MGT-341; Dis. Preparedness Hosp/HC | Fox Valley Tech T.C. | July 26-27 | https://my.teex.org/TeexPortal/Default.aspx?MO=mCourseCatalog&D=EU&C=MGT341&S=476 |
| CISM – Group | Columbia Sheriff Office | June 17-18 | Contact HERC coordinator |
| AWR-331; Winter Weather | Lincoln County | 27-Sep | https://ndptc.hawaii.edu/training/delivery/3120/ |
| AWR-232; Mass Fatalities Planning | Oneida County Sheriff | 29-Jun |
SCWIHERC Exercises
-Medical Response Surge Exercise – Replaces Coalition Surge Test. Planning to start this summer. Tie into DARES scenario?
-Pediatric Surge TTX – As part of MRSE exercise/scenario?
Annual Plans Review:
After plans are reviewed and updated, Docusign process, same as last year. Sent to every core organization except EMS (which will be sent June 16), signatures due by June 30.
Scholarships:
Scholarship opportunities start July 1! $2,000 aggregate limit per active member (must provide proof of participation in 2 SCWIHERC events in previous 365 day period), must meet other application requirements. Valid on conference registration fees, travel (mileage/flight/lodging). Scholarship opportunity excludes PHEP recipients, please use PHEP funds!
Burn Surge Plan Review and Tabletop Exercise: SitMan and slides available in Shared Drive, also review recording.
Hospital Meeting:
ABLS:
Is a mess, please continue to send your registered student information, please be patient and standby! Student will receive an email when successfully enrolled and course is accessible.
SALT Triage First Receiver Train the Trainer
Resuming this project after COVID delay. Three facets of training/maintaining staff proficiency:
- SALT Triage First Receiver video, which should be viewed by anyone in your organization who might be put to the task of triage in the event that you have an MCI in your community that would result in self-presenting patients. Link: https://youtu.be/N7OG8a7vXnE
- Train the Trainer sessions for our Champions to review the concepts and receive training on our SALT ribbon bags, see emailed out April 27. We will distribute the ribbon bags for your facility to your Champion at these trainings.
- Your Champions bring their training and ribbon bags back to your facility, where they train your other staff on these SALT triage concepts, and how to use the ribbon bags, and maintain a regular competency program for your new hires and as part of annual training for current staff.
About half of hospitals have received their bags and participated in our SCWIHERC trainings in mid-May. Direct outreach to hospitals that haven’t is forthcoming. We really encourage all of our regional hospitals to join this project to ensure they have staff that know how to field triage self-presenting patients and their triage methods are consistent with EMS field triage.
CSC Updates: Doug Hill
Wisconsin Hospital Mutual Aid MOU- There is not a strong statewide desire to renew this document as a state. Opportunity to develop regional MOUs if desired, (what are next steps/follow up?)
CSC Concept of Operations- Doug Hill is developing as part of grant deliverables, but it leans more along the lines of allocation of scarce resources than crisis standards of care.
CSC Article: https://www.tandfonline.com/doi/full/10.1080/15265161.2021.1925778 PDF of article available in Best Practices Folder of shared drive.
GE IV Contrast Shortage- Looks like we’re coming out of it. No current concerns.
TJC EM Standards Update Resources:
From Wakefield Brunswick:
AHEPP Webinar June 15 1100 recording will be posted to notes at http://www.scwiherc.org/june-15-2022-membership-meeting/ when available.
Lessons Learned and Best Practices from COVID-19 and other real events:
How are we remaining nimble for future variants/surge/vaccination/testing?
What else are we working on? Mass casualty drills, implementing SALT Triage in ED.
What else are we responding to? Current event in Dane County from June 13 storm, widespread power outages including some persisting into 48+ hours (as of the time of these notes being written). Compounded by heat advisory. More widespread severe storms anticipated tonight through whole region and state, be prepared! Current lessons learned: cell networks were jammed immediately after power outage, don’t forget basics like Wireless Priority Service, WISCOM radio, GETS cards, FirstNet. When SCWIHERC Responder has communication issues (Jennifer lost power during event and cell service was spotty for a few hours), that will be posted on EMResource under coalition header at top of page (hover over Jennifer’s name), and as out of office reply on email when possible, with further instruction.
Meeting Attendance:
Jane Lentz-Gervais- Adams County EM
Charlie Johnson- St. Mary’s Madison
Jeff Kindrai- Grant County HD
Brent Skiba- Watertown Regional Medical Center
Mike Tedeschi- NEWHERC
Lisa Herritz- Ho Chunk Nation
Joe Meagher- Dodge County EM
Jennylynde Packham- UW Health Rehab
Dave Kitkowski- St. Clare Baraboo
Katie Budack- Grant Regional Health Center
Matt Christian- Marshfield Medical Center Beaver Dam
Angie Cohen- Grant Regional Health Center
Doug Hill- CSC Coordinator
Tina Strandlie- Stoughton Health
Bill Ritzer- Reedsburg Area Medical Center
Galen Kennedy
Kara Takes- Unified Therapy
Diana Quinn- SSM Health
Lynn Skatrud- Green County HD
Michael Niles- Rock County HD
Nathan Bubenzer- UPH Meriter
Ed Somers Clearview Dodge County
Suzanne Schreiner- Adams County HHS
Rodney Punzel- UW Health
Julie Gorman- Sauk Prairie Healthcare
Jodie Molitor- Sauk County HD
Jen Hankwitz- UW Health
Brian Allen- Southwest Health
Michael Stephens- UW Health
Alice Salli- Mendota Mental Health Institute
Sam LaMuro- Fort HealthCare
Mary Tessendorf- Monroe Hospital
Steve Haskell- UW Health
Jim Abitz- Southwest Health
Carol Brown- Rainbow Hospice
Jennifer Lorenz- Mercyhealth Janesville
Kurt Hoeper- Upland Hills Health
Sarah Jensen- Marquette County HD
Sally Blackbourn- Memorial Hospital of Lafayette County
Lori Mickelson- UW Health Burn Program
Carmen Carpenter
Mike Hall- Monroe Hospital
Dave Larson- Madison VA
Dr. Mike Lohmeier- SCWIHERC
Jennifer Behnke- SCWIHERC
May 3, 2022 Membership Meeting
Join us for our membership meeting May 3: https://us06web.zoom.us/j/83510672818?pwd=eE9HcXBPNVhxVVdHUGJBbUxlRFVEdz09
Agenda:
May 3 2022 Membership Agenda
May 3 SCWIHERC Membership Meeting Notes
Recording:
Passcode: refer to email from May 3 or ask Jennifer
Reminder that COVID AAR survey is due May 27, see email sent April 23 for more info and link to survey.
Upcoming Trainings and Information:
| Course | Location | Date | Link if available |
| MGT-341; Dis. Preparedness Hosp/HC | Spooner | October (TEEX still determining exact date) | |
| MGT-341; Dis. Preparedness Hosp/HC | Fox Valley Tech T.C. | July 26-27 | https://my.teex.org/TeexPortal/Default.aspx?MO=mCourseCatalog&D=EU&C=MGT341&S=476 |
| CHEC – Basic & Advanced | Wausau | May 17-19 | Contact HERC coordinator |
| CISM – Group | Columbia Sheriff Office | June 17-18 | Contact HERC coordinator |
| AWR-331; Winter Weather | Lincoln County | 27-Sep | https://ndptc.hawaii.edu/training/delivery/3120/ |
| AWR-232; Mass Fatalities Planning | Oneida County Sheriff | 29-Jun | |
| AWR-326; Tornado Awareness | Lake Delton | 17-May | https://ndptc.hawaii.edu/training/delivery/3119/ |
| MGT-439; Pediatric Disaster Response | Milwaukee | May 5 – 6 | Pediatric Disaster Response and Emergency Preparedness | TEEX.ORG |
SCWIHERC Exercises
-Burn Surge TTX Due June 30 – Scheduled for NEXT SCWIHERC MEETING (Date TBD soon)
-Medical Response Surge Exercise – Replaces Coalition Surge Test. Likely this summer. Tie into DARES scenario?
-Pediatric Surge TTX – As part of MRSE exercise/scenario?
Annual Plans Review:
After plans are reviewed and updated, Docusign process, same as last year. Goal to send out at beginning of June, signatures due by June 30.
ABLS:
Is a mess, please continue to send your registered student information, please be patient and standby! Student will receive an email when successfully enrolled and course is accessible.
SALT Triage First Receiver Train the Trainer
Resuming this project after COVID delay. Three facets of training/maintaining staff proficiency:
- SALT Triage First Receiver video, which should be viewed by anyone in your organization who might be put to the task of triage in the event that you have an MCI in your community that would result in self-presenting patients. Link: https://youtu.be/N7OG8a7vXnE
- Train the Trainer sessions for our Champions to review the concepts and receive training on our SALT ribbon bags, see emailed out April 27. We will distribute the ribbon bags for your facility to your Champion at these trainings.
- Your Champions bring their training and ribbon bags back to your facility, where they train your other staff on these SALT triage concepts, and how to use the ribbon bags, and maintain a regular competency program for your new hires and as part of annual training for current staff.
Lessons Learned and Best Practices from COVID-19 and other real events:
How are we remaining nimble for future variants/surge/vaccination/testing?
Hospitals: creation of a high consequence infectious disease plan/annex at the hospital level that details information regarding medical countermeasures, Strategic National Stockpile, volunteer management (including WEAVR), ASPR pandemic preparedness checklist (https://files.asprtracie.hhs.gov/documents/aspr-tracie-hcc-pandemic-checklist-508.pdf), PPE burn rate calculator (https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/burn-calculator.html), Acute Hospital Care at Home (see COVID-19 email update sent April 1), other healthcare at home initiatives. Integrating COVID population back into hospital units (in negative pressure rooms) to free up COVID units but maintain them for additional surge readiness.
Local Health Departments: maintaining capacity for contact tracing, testing, and vaccination, cross training staff on all so they can meet current needs. Maintaining testing capacity with state contracts and private testing vendors. Continue to meet with healthcare partners to maintain readiness.
Other Healthcare providers: continuing to practice good infection control practices including masking per CDC guidelines (https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html), working with local pharmacies to maintain testing and vaccination capacity
What else are we working on? Workplace violence training/escaping violent encounters, missing persons drills, hospital evacuation training, streamlining plain language alerts (getting away from code colors). Public health also working on responding to higher rates of other communicable diseases, boosting childhood vaccination rates that have suffered during pandemic by promoting Vaccines for Children providers/enrollment, lead screening, home visits, starting WIC in person again.
We could do better on EMResource response rates, especially for MCI events. Response to these alerts breaks down based on a number of factors, including staff turnover and not being able to keep up with training, how alerts are received, alert fatigue, being able to tell from an alert if something is informational only or requires action. Will take back to discuss further at state level. EMResource resources are available in SCWIHERC shared drive -> EMResource. Additional information and resources: https://www.dhs.wisconsin.gov/preparedness/systems/emresource.htm Reach out to Jennifer to troubleshoot/verify alerts/facilitate training.
Brian Kaczmarski, Statewide HERC Coordinator, gave a presentation on the state and regional High Consequence Infectious Disease Plans. The current version of these plans as well as the slides from the presentation are available in the shared drive. A resource mentioned during the presentation is the Dane County EMS Primer on Infectious Disease: https://em.countyofdane.com/documents/pdfs/ems/Infection-Control-EMS-Primer-on-ID-7.11.19.pdf
We then transitioned into a tabletop exercise/discussion on a High Consequence Infectious Disease scenario. The Situation Manual for this exercise is available in the SCWIHERC shared drive ->Exercise Templates.
Meeting Attendance:
Josh Kowalke- Reedsburg Ambulance
Emily Kosterman- Waupun Memorial
Jeff Kindrai- Grant County Health Dept
Jodi Moyer- Beloit Memorial
Lynn Skatrud- Green County Health Dept
Elizabeth Chilsen- Jefferson County Health Dept
Lisa Herritz- Ho Chunk Nation Health
Andy Koehler- Fort Health Care
Angie Cohen- Grant Regional
Sam LaMuro- Fort Health Care
Jodie Molitor- Sauk County Health Dept
Tina Strandlie- Stoughton Health
Lyle Kratochwill- Richland Hospital
Jennylynde Packham- UW Health Rehab
Sarah Jensen- Marquette County Health Dept
Christal Foreyt- Gundersen Boscobel
Sarah Van Hoof- UW Health
Jessie Phalen- Sauk County Health Dept
Dave Kitkowski- SSM Health St. Clare Baraboo
Nikki Ripp- Adams County Health Dept
Tanna McKeon- Green County EM
Kara Takes- Unified Therapy
Michael Guss- Walworth County Health Dept
Dave Larson- Madison VA
Mike Stephens- UW Health
Lori Mertens Pelleteri- SSM Health
Brenda Totzke- Mile Bluff Medical Center
Sally Blackbourn- Memorial Hospital of Lafayette County
Mary Bender
Kelly Mitchell- UW Health
Ken Van Horn- Public Health Madison and Dane County
Carmen Carpenter- Iowa County Health Dept
Steve Haskell- UW Health
Aurielle Smith- SCWIHERC and PHMDC
Victoria Parker- Watertown Health Dept
Katie Budack- Grant Regional
Michael Niles- Rock County Health Dept
Kurt Hoeper- Upland Hills Health
Julie Gorman- Sauk Prairie Healthcare
Karen Sell- Prairie Ridge Health Columbus
Tammy Kingery- Gundersen Moundview
Jane Lentz-Gervais- Adams County EM
Brianna Juszczak- Mile Bluff Medical Center
Heidi Finucan- Mile Bluff Medical Center
Diana Quinn- SSM Health
Donna Haugom- Jefferson County Emergency Management
Julie Leibfried- Lafayette County Health Dept
Samroz Jakvani- Jefferson County Health Dept
Brian Kaczmarski- WI HERCs
Jennifer Behnke- SCWIHERC
SCWIHERC Network Recovery Exercise April 12
Our Network Recovery Exercise took place on April 12, thank you for your participation. The After Action Report and Improvement Plan will be shared when it is available.
December 1, 2021 Membership Meeting
December 1 SCWIHERC Membership Meeting Notes
Meeting Recording Link (will expire November 30, 2022): https://transcripts.gotomeeting.com/#/s/5cf0be5de39db689f4f6e1cb48dd4a53eeef6f86fa0aa3509f3d0de1a9bf5793
We started by reviewing EMResource user info and event notification preferences. Both of these are found under the “Preferences” tab. It is recommended that your ED HUC desk landline number be added to the EM Coordinator’s EMResource notification voice section under “Preferences” and “User info.” Remember to click save when navigating away from this form. Then go into event notifications and check the voice box for MCI region 5, MCI statewide/bordering regions, Bed Count region 5, Bed Count Statewide/bordering regions, general announcement region 5 and statewide/bordering regions, and any other alerts you want the ED to receive. Click save when navigating away from this form. Be sure the EM Coordinator and any other appropriate users are receiving other important notifications such as resource request, be on the look out, Amber alert, etc. Note that we have recently noted serious delays in notifications coming from certain events (seems to be tied to general announcement type events) and an escalated support ticket has been started with Juvare.
Anyone needing help setting up or verifying alerts, or refresher EMResource training with staff, should reach out to Jennifer.
We discussed the Regional Medical Coordination Center concept. Any time an incident happens within SCWIHERC’s 14 county region, we may activate the RMCC to help the field determine where to transport patients from the field. The recommended threshold for activation is 5 patients or more. It is critical for hospitals to respond to the MCI alert within 15 minutes. This helps the field help your facility by trying not to give you more than you can handle, which is important with high census right now. If the needs of the field can’t be met with the numbers currently entered, you may be asked to refresh your bed counts accordingly. Please also be aware that the field may send you at least one patient prior to receiving counts, which is also why your response is important. If there is an MCI close to your facility, your facility should always expect to receive some patients from that scene.
We reviewed the EmPOWER and Social Vulnerability Index data. Jennifer sent out the most recent update on October 20. It is a grant deliverable to send this out twice a year. There is a summary of numbers of electricity-dependent CMS beneficiaries broken down by county in this update, and there is a new spreadsheet that breaks out those beneficiaries based on categories like ventilators, oxygen tanks or concentrators, dialysis, electric mobility devices etc. The spreadsheet contains tons of information and definitions. These numbers are helpful for planning and should be shared with local planning partners. The limitation to this data is it is all de-identified, so it doesn’t help us find these populations until after an emergency has occurred, therefore we don’t know how to use this list to the greatest benefit of our communities. There are opportunities for whole community preparedness and collaboration with other providers, such as home health and hospice agencies, dialysis and durable medical equipment providers, to better prepare for caring for these populations.
General EmPOWER data can be found at: https://empowermap.hhs.gov/
The EmPOWER spreadsheet is obtained from HHS and uploaded to the PCA Portal where Health Departments and HERC Coordinators can retrieve it.
Social Vulnerability Index data is at https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
Including county level data: https://svi.cdc.gov/prepared-county-maps.html
We had a discussion on several topics related to COVID-19 response:
Questions on how orgs are adapting their ICS structure to such a long event: holding meetings virtually, relying on dashboards for info sharing, moving to weekly meetings.
Questions on how orgs are managing their AAR process: several subsections or versions of AAR to cover different phases of pandemic.
Discussion around current visitor policies: only allowing one visitor at a time, in some cases only one visitor per day (same person can come and go, but multiple visitors cannot). Some variation with OB, PEDs, and end of life patients. Offering or requiring visitors wear masks. No visitors for COVID positives or respiratory patients until COVID ruled out. Meriter shared external link to their policies: https://www.unitypoint.org/madison/coronavirus-updates-closings.aspx
Lots of discussion on how visitor policies have led to an increase in security and behavioral events due to visitors’ unwillingness to comply.
General discussion around coping with surge. Facility closed urgent care to move staff to ED, but caused an uptick in ED visits. Biggest barriers are staffing shortage, lack of physical room, extended wait for transfers, lack of transportation options. Question on using Critical Care Paramedics to augment Respiratory Therapy in hospitals? Also still asking for another ACF to decompress surge.
Shortage of post-acute care available beds, including noting problems with major variations from one facility to another in admission parameters (COVID history, how many days since COVID negative, patient can’t have visitors for 90 days after COVID (note that prohibiting visitors is not allowed and addressed by CMS here: https://www.cms.gov/files/document/qso-20-39-nh-revised.pdf)
Also don’t forget RAST resource for helping LTCF with outbreaks: https://www.dhs.wisconsin.gov/publications/p02883.pdf
Joe Cordova reviewed the resources for staffing assistance. This process will be coming down officially in writing, but consists of: 2 attempts at WEAVR outreach (first doesn’t yield much, sometimes second does) WEAVR request procedure: https://content.govdelivery.com/accounts/WIDHS/bulletins/2f696ca. WI DHS staffing resource assistance (Jennifer emailed on Oct 1). If those resources aren’t sufficient, email Joe (joseph.cordova@wi.gov) to discuss the process of applying for federal staffing assistance (Jennifer emailed the form and additional FEMA information to hospitals on November 20. Do not submit this form to your local Emergency Manager, email Joe with questions). Note that federal staffing requests are usually only granted for 2-3 week deployments, and that FEMA will want requestors to provide details both on how staff will be used, and what the facility’s plan for staffing is once the deployment, if granted, ends.
Finally, we shared identified needs and ideas for supporting staff mental health and resiliency. With staffing being one of our biggest limiting factors, and staff burnout being one of the biggest causes, providing staff support should be an organizational priority.
Ideas shared include giving staff the opportunity to share their stories and know that they are not alone. Having separate support groups for leadership where they can feel vulnerable. Manager purchased the book ER Nurses by James Patterson and wrote a message of appreciation and admiration for each of them inside. Offering support groups to staff. Deployed a therapist to round on units for staff. Hospital wellness coordinator shared materials and resources, Jennifer will try to get and share. “Managing the soft side of hard stuff.” Jennifer shared debriefing that another colleague did for HERC staff, will look at SCWIHERC offering that in an anonymous and virtual environment where staff can just drop in and talk with their peers from outside their organization. Will look at providing a separate offering for leaders so they have a safe space to feel vulnerable outside their normal management duties.
SCWIHERC Deliverables/Projects Update agenda item was not covered due to lack of time, will be covered at a future meeting.
Meeting attendance:
Chad Atkinson- Mercyhealth
Jeff Ethington- UW Health OPO
Joe Meagher- Dodge County EM
Diana Quinn- SSM Health
Lisa Herritz- Ho Chunk Nation
Steve Haskell- UW Health
Sharon Warden- Mile Bluff Medical Center
Kara T-Unified Therapy
Lori Mertens Pelliteri- SSM Health
Alice Salli- Mendota Mental Health
Mary Tessendorf- Monroe Hospital
Aurielle Smith- SCWIHERC and Public Health Madison Dane County
Jane Gervais- Adams Co EM
Mike Hall- Monroe Hospital
Tom Ellison- UW Health
Dave Larson- Madison VA
Asa Rowan- Beloit Area Community Health Systems
Jodie Molitor- Sauk Co HD
Kurt Hoeper- Upland Hills Health
Gail Scott- Jefferson Co HD
Bob Swenarski- St. Mary’s Janesville
Allison Davey- Green Lake Co HD
Keith Hurlbert- Iowa Co EM
Kathy Johnson- Columbia Co EM
Angie Cohen- Grant Regional Health Center
Tina Strandlie- Stoughton Health
Sarah Jensen- Marquette Co HD
Sam LaMuro- Fort Health Care
Amy Nehls- Dodge Co EM
Jeff Kindrai- Grant Co EM
Matt Byczek- UnityPoint Health
Jessie Phalen- Sauk Co HD
Ron Krause- Mercyhealth
Brenda Koehler-Borchardt- Watertown Regional Medical Center
Amanda Dederich- Juneau Co HD
Angie Zastrow- Rainbow Hospice
Laura Kane- UW Health
Josh Kowalke- Reedsburg Ambulance
Katrina Harwood- Rock Co HD
Christal Foreyt- Gundersen Boscobel
Suzanne Schreiner- Adams Co HD
Nathan Bubenzer- UPH Meriter
Carrie Meier- Dane Co EM
Julie Gorman- Sauk Prairie Healthcare
Brian Allen- Southwest Health
Samroz Jakvani- Jefferson Co HD
Megan Lee- UW Health
Russ Sprecher- St Clare Meadows
Julie Liebfried- Lafayette Co HD
Mike Stephens- UW Health
Michael Niles- Rock Co HD
Joe Cordova- WI DHS
Jennifer Behnke- SCWIHERC
SCWIHERC Hospitals See High Patient Volumes, Limited Resources – News Release
FOR IMMEDIATE RELEASE
September 10, 2021
Hospitals in South Central Wisconsin see high patient volumes, limited resources
Hospitals seek community help to prevent COVID-19 cases putting critical strain on regional healthcare systems
Hospitals and healthcare facilities throughout southcentral Wisconsin are experiencing a high volume of inpatients, limiting hospital beds and putting a strain on resources.
This serious situation is occurring across the 14 counties of the South Central Wisconsin Healthcare Emergency Readiness Coalition, (SCWIHERC). Its member hospitals are asking for our communities’ help.
To better control the situation, the hospitals are urging everyone to continue being vigilant with COVID-19 safety measures, such as receiving any COVID-19 vaccine, masking, and physically distancing where appropriate.
This present high volume of patients spans across critical care areas of the hospitals, like intensive care units (ICU), general medical floors, and emergency departments. With resources stretched, it is becoming more difficult to receive care close to home if you may need it for COVID and non-COVID-related illnesses.
From July 28 to Sept. 1, the total number of COVID-19 hospitalizations increased four-fold in the South Central region. In that same timeframe, there were 5.5 times the number COVID-19 ICU hospitalizations. Many rural hospitals have no or limited ICU capability and are all reliant on the same limited ICU beds in larger cities, including Madison.
While the current high volume in healthcare facilities in the region is a mixture of COVID-19 and non-COVID-19 patients, a rise in preventable COVID-19 admissions is a driving factor. Preventing a further rise in COVID-19 admissions is our focus in this critical time.
In fact, COVID-19 infections requiring hospitalization are increasing at a similar rate to last winter’s surge. With students from pre-K through college returning to classrooms, the Labor Day holiday, and colder weather soon driving people indoors, additional increases are expected which could stretch resources to critical levels.
To receive a COVID-19 vaccine, please contact your local healthcare providers, or visit the state Department of Health Services vaccine webpage.
###
The South Central Wisconsin Healthcare Emergency Readiness Coalition (SCWIHERC) is a coalition that collaborates with 29 area hospitals and numerous other healthcare providers over 14 counties to prepare for and respond to emergencies in South Central Wisconsin.
SCWIHERC Members signing this message:
| Organization | Media Contact Name and Email (if provided) |
| South Central Wisconsin Healthcare Emergency Readiness Coalition | Jennifer Behnke (jennifer.behnke@scwiherc.org) |
| Aspirus Divine Savior Hospital and Clinics | Haley Gilman (haley.gilman@aspirus.org) |
| Beloit Health System | Megan Goggin (mgoggin@beloithealthsystem.org) |
| Edgerton Hospital and Health Services | |
| Grant Regional Health Center | |
| Gundersen Health System | Chris Stauffer (cjstauff@gundersenhealth.org) |
| Marshfield Medical Center – Beaver Dam | Dan Baulch (baulch.dan@marshfieldclinic.org) |
| Memorial Hospital of Lafayette County and Primary Care Clinics | |
| Mercyhealth | Rebecca Rose (rrose@mhemail.org) |
| Mile Bluff Medical Center, Mauston | |
| Prairie Ridge Health | |
| Reedsburg Area Medical Center | Robert Van Meeteren (rvanmeeteren@ramchealth.org) |
| The Richland Hospital | Lyle Kratochwill (lyle.kratochwill@richlandhospital.com) |
| Sauk Prairie Healthcare | Amy Ryan (amy.ryan@saukprairiehealthcare.org) |
| SSM Health | Lisa Adams (Lisa.Adams@ssmhealth.com) |
| Southwest Health | Jaime Collins (collinsj@southwesthealth.org) |
| Stoughton Health | Laura Mays (lmays@stoughtonhealth.com) |
| UnityPoint Health – Meriter | Nicole Aimone (Nicole.Aimone@unitypoint.org) |
| UW Health | Andrew Hellpap (AHellpap@uwhealth.org) |
| Watertown Regional Medical Center | Steve Hunt (Steven.Hunt@watertownregional.com) |
| William S. Middleton Memorial Veterans Hospital | Paul Rickert (paul.rickert@va.gov) |